Anatomy of The Inguinal Region
- What is the inguinal region and why is it important?
- Difficulties in Understanding Inguinal Anatomy
- Inguinal Region Anatomy (Anterior View)
- Inguinal Hernias
- Encyclopedia of the Inguinal Region
- Structures Originating from the Superficial Fascias (Camper and Scarpa)
- Camper's Fascia
- Scarpa's Fascia
- Buck's Fascia
- Tunica Dartos
- Colles' Fascia
- Structures Originating from the External Oblique Muscle Aponeurosis
- Inguinal Ligament (Poupart's Ligament)
- Lacunar Ligament (Gimbernat's Ligament)
- Reflected Ligament (Ligamentum Reflexum, Colles' Ligament, Fascia Triangularis Abdominis, Triangular Fascia)
- Pectineal Ligament (Cooper's Ligament)
- Conjoint Tendon (Henle’s Ligament, Inguinal Falx, Inguinal Aponeurotic Falx)
- Interfoveolar Ligament
- Iliopubic Tract
- Spermatic Cord Contents (Structures)
- Ductus Deferens
- Pampiniform Plexus
- Gonadal Arteries
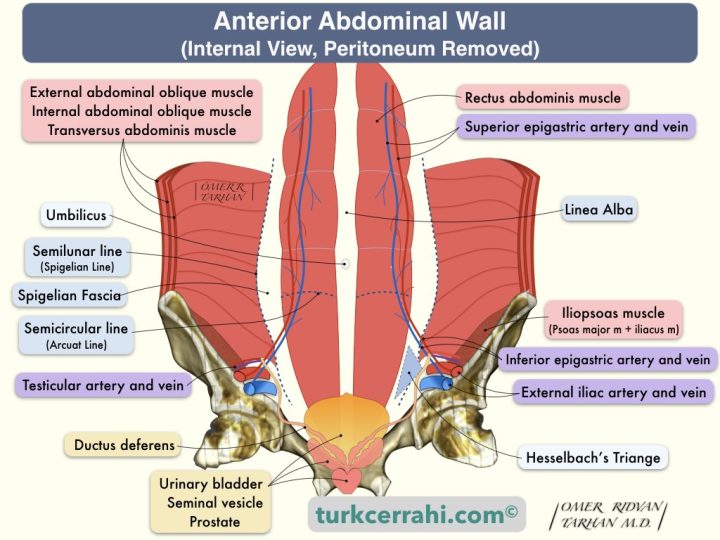
- Arcuate Line (Semicircular Line (of Douglas))
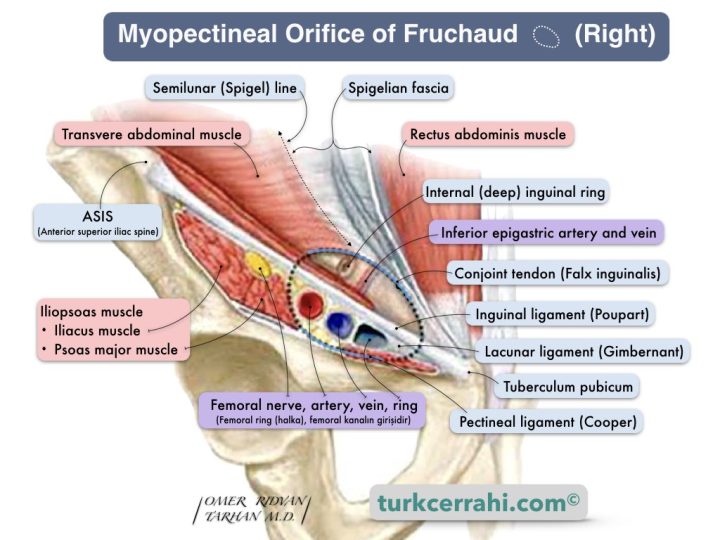
- Semilunar Line (Spigelian Line), Spigelian Fascia and Spigelian Hernia
- Structures Originating from the Superficial Fascias (Camper and Scarpa)
1. What is the inguinal region and why is it important?
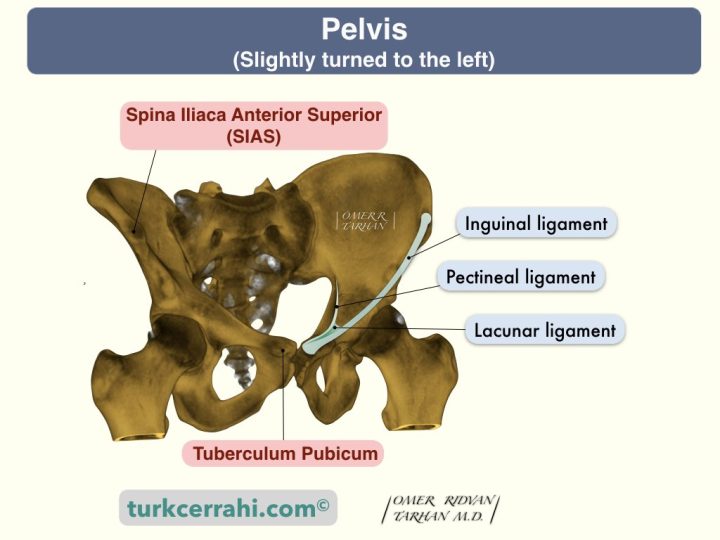
The groin, or inguinal region, is the depressed area between the abdomen and the thigh that is bounded medially by the pubic tubercle and superolaterally by the ASIS (anterior superior iliac spine).
The inguinal region is the right and left lower parts of the anterior abdominal wall in the nine-region organization. The terms "groin" and "inguinal region" are used interchangeably or synonymously.
The groin contains an imaginary canal called the inguinal canal. The inguinal region is the weakest point in the abdominal wall. Consequently, it is prone to hernia formation.
There are two types of inguinal hernias: direct and indirect.
A direct hernia is a hernia that protrudes directly from the abdominal wall. Direct inguinal hernias are located medial to the inguinal canal and inferior epigastric artery.
On the other hand, indirect inguinal hernias pass through the inguinal canal, exit the superficial inguinal ring, and may continue into the scrotum or labia majora.
Direct inguinal hernias do not descend into the scrotum because they aren’t inside the inguinal canal. With careful examination, we can distinguish between the two.
2. Difficulties in Understanding Inguinal Anatomy
Imaginary Structures
The structures are beautifully illustrated in anatomy books. However, neither the definitions nor the drawings match the appearance of the surgery.
Inguinal Canal
For example, the term “inguinal canal” evokes a tubular structure of connective tissue. In reality, the inguinal canal is a transition zone for various structures that pass between the abdomen and the scrotal structures (i.e., the spermatic cord and round ligament).
During fetal development, the testicles form in the abdomen and move through the inguinal canal to the scrotum in the last few months of development.
The inguinal canal is imaginary. The inguinal canal is a passage located in the lower part of the groin and is the site where the spermatic cord passes through in males and the round ligament passes through in females. The walls of the inguinal canal are formed by tissues surrounding the spermatic cord or round ligament. These walls include the roof (above), floor (below), anterior (front), and posterior (back) aspects of the canal.
Conjoint (Conjoined) Tendon
The structure called the conjoined tendon is often not a visible structure like the Achilles tendon.
The conjoint tendon is considered a structure formed from the lower part of the common aponeurosis of the internal oblique muscle and the transversus abdominis. However, this aponeurotic structure can be seen in half or less of the patients. The conjoint tendon is frequently largely muscular rather than aponeurotic. Therefore, it may be more reasonable to view the conjoint tendon as the common lower edge of the two muscles. Conjoint tendon is also called the inguinal falx.
Structures with Multiple Names
Almost every structure in the inguinal region has at least two names.
Examples
- Inguinal ligament = Poupart's ligament, groin ligament
- Cooper’s ligament= Pectineal ligament
- Gimbernat’s ligament=Lacunar ligament
- Conjoint tendon= Inguinal falx,iInguinal aponeurotic falx, conjoined tendon, Henle’s Ligament
- Reflected Ligament=Ligamentum Reflexum, Colles' Ligament, Fascia Triangularis Abdominis, Triangular Fascia
- Interfoveolar Ligament=Hesselbach's Ligament)
The Presence of Dozens of Structures within a Hand Palm-Sized Area
Structures within the spermatic cord and the nerves, ligaments, and vessels in this region.
3 Dimensionality
Viewing the inguinal anatomy both anteriorly and posteriorly complicates the issue. While the anterior view is important for open surgery, the posterior view is important for laparoscopic surgery.
Drawings by Different Artists in the Same Article
In articles concerning inguinal anatomy or hernias, drawings from different sources and artists, different perspectives, and different details also make it difficult to understand groin anatomy.
Asymmetrical Drawings
To show many things in one image, illustrating different layers on the right and left sides creates adaptation problems, especially for new learners.
3. Inguinal Region Anatomy (Anterior View)
Under the skin is the superficial fascia (subcutaneous adipose tissue, or SAT). The superficial fascia is a single layer above the umbilicus, divided into two layers below the umbilicus: the superficial layer (Camper’s fascia) and the deep layer (Scarpa’s fascia).
The superficial layer of the superficial fascia (Camper's fascia) is fatty and thin on the upper part of the abdomen and thicker on the lower part.
The deep layer of the superficial fascia (Scarpa fascia) is membranous and contains little or no fat.
The external oblique muscle aponeurosis is situated beneath the subcutaneous adipose tissue (superficial fascia) in the inguinal region. It also forms the anterior wall of the inguinal canal.
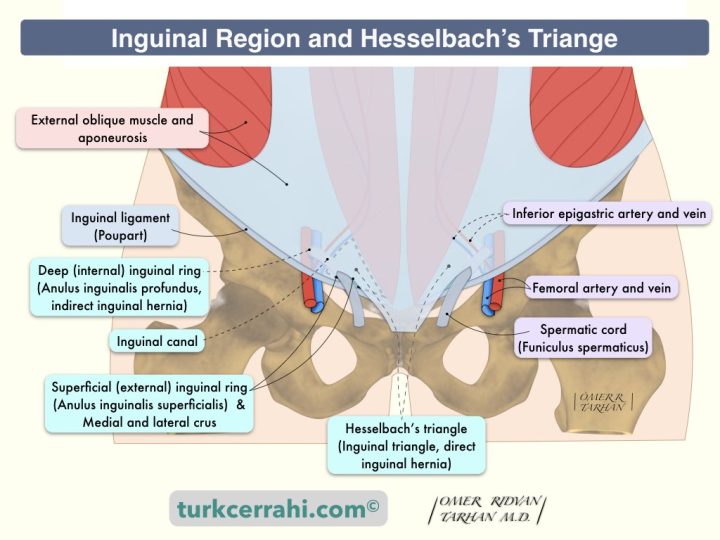
Inguinal Canal
The inguinal canal is an oblique passage through the lower abdominal wall that is located just above and parallel to the inguinal ligament. It is a canal through which the spermatic cord passes in males and the round ligament of the uterus in females. It is about 4 cm long. Two openings at the beginning and end of this channel are called the deep inguinal ring and superficial inguinal ring, respectively.
- The deep inguinal ring is also called the internal inguinal ring or anulus inguinalis profundus.
- The superficial inguinal ring is also called the internal inguinal ring or anulus inguinalis superficialis.
The inguinal canal is an imaginary canal where the spermatic cord (funiculus spermaticus) passes in males and the round ligament (ligamentum teres uteri) in females.
Spermatic Cord (Funiculus Spermaticus)
It contains structures that connect the testes to the abdominal cavity.
Contents of Spermatic Cord
- Vas (ductus) deferens (seminal duct)
- Vessels
- Testicular artery (from the abdominal aorta)
- Pampiniform plexus (testicular veins)
- Deferential artery (=arteria ductus deferens, branch of the superior vesical artery)
- Cremasteric artery and vein (=external spermatic artery and vein)
- Nerves
- Genital branch of genitofemoral nerve (innervates cremaster muscle)
- Sympathetic and visceral afferent fibers
- İlioinguinal nerve
- Lymphatics
- Remnants of the vaginal process (processus vaginalis)
Structures Covering the Spermatic Cord (Outside to Inside)
- External spermatic fascia (extension of external oblique muscle aponeurosis)
- The cremasteric fascia (including the cremasteric muscle) is an extension of the internal oblique muscle and aponeurosis.
- Internal spermatic fascia (extension of transversalis fascia)
Round Ligament of Uterus (Ligamentum Teres Uteri)
It is a cord-like structure that emerges from the uterus (uterine horn). After passing through the inguinal canal, it comes to the labium majus and disperses and integrates with the connective tissue there. The function of the round ligament is to maintain the anteversion of the uterus by pulling the fundus forward during pregnancy. It can be cut and removed in hernia surgeries.
The Walls of the Inguinal Canal
(Anatomic relations of Spermatic cord or Round Ligament or Surrounding Structures)
1. Anterior Wall
The anterior wall of the inguinal canal is formed by the external oblique aponeurosis. (The lower fibers of the internal oblique muscle enter between the cord and the external oblique fascia, strengthening the posterior wall and the inner ring in this region.)
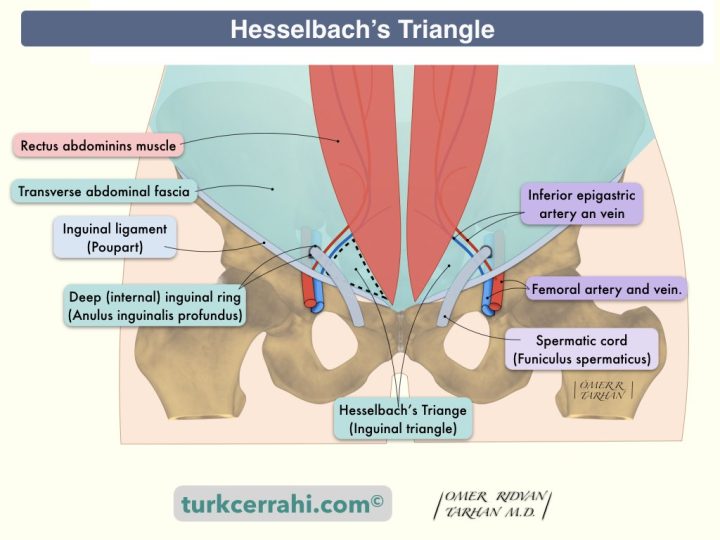
2. Posterior Wall
The posterior wall of the inguinal canal is formed by the transversalis fascia. (in the medial third of the posterior wall, the tendon conjoint (inguinal falx) insert between the cord and the transversalis fascia, strengthening this part of the posterior wall.)
3. Roof
The roof of the inguinal canal is formed by the lower fibers of both the internal oblique and transversus abdominis muscles. These fibers start from the inguinal ligament and are muscular laterally. They then transform into fascia medially to form the tendon conjoint (inguinal falx) and attach to the pubic crest and pectineal line of the pubis.
4. Floor
The floor of the inguinal canal is formed by the medial third of the inguinal ligament (Poupart ligament). The inguinal ligament is the thickened lower edge of the external oblique muscle aponeurosis. It attaches to the anterior superior iliac spine superiorly and the pubic tubercle inferiorly. The inguinal canal floor is reinforced medially by the lacunar ligament and laterally by the iliopubic tract.
Deep (Internal) Inguinal Ring (Anulus Inguinalis Profundus)
The deep (internal) inguinal ring is the entrance to the inguinal canal. It is in the middle of the distance between the anterior superior iliac spine and the pubic symphysis. It is just above the inguinal ligament and lateral to the inferior epigastric vessels. According to some, the deep inguinal ring is an opening in the transversalis fascia, while others believe it is a tubular extension of the transversalis fascia, covering the internal spermatic fascia of the spermatic cord in the male and the outer layer of the round ligament of the uterus in the female.
Superficial (External) Inguinal Ring (Anulus Inguinalis Superficialis)
The superficial (external) inguinal ring is just above the pubic tubercle. Although it is called the outer ring, it is actually a triangle. The external inguinal ring is in the lower part of the external oblique muscle aponeurosis. The two sides of the triangle are called the medial and lateral crus (attached to the pubic symphysis and pubic tubercle, respectively). The transverse fibers that prevent tearing the top of the triangle are called intercrural fibers. The fibers of the external oblique muscle aponeurosis that emerge from the external ring surround the funiculus spermaticus, and it is referred to as the external spermatic fascia.
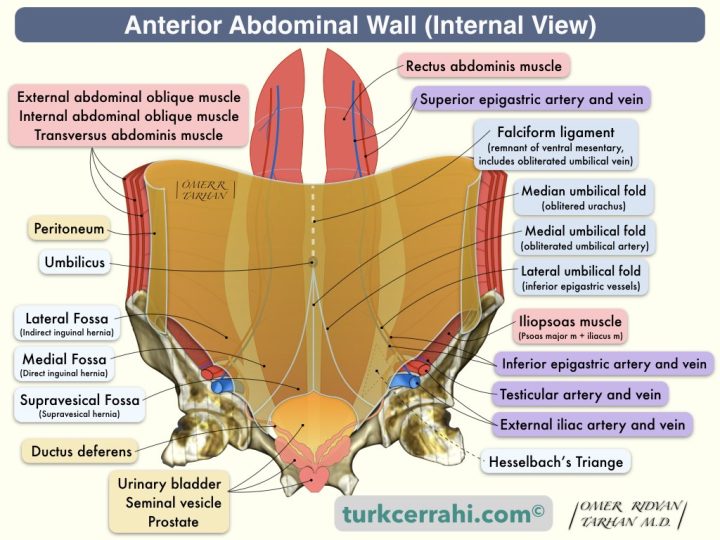
Hesselbach's Triangle
(Inguinal Triangle, Franz Kaspar Hesselbach, German surgeon anatomist, 1759-1816)
Hesselbach's Triangle is the region where direct inguinal hernias arise. Hesselbach's Triangle corresponds to the medial inguinal fossa when viewed from inside the groin.
Boundaries of Hesselbach's Triangle
- Lateral: Inferior epigastric artery
- Medial: Rectus abdominis muscle
- Inferior: Inguinal ligament
4. Inguinal Hernias
Inguinal hernias are the protrusion of a peritoneal sac through the inguinal region, the abdominal wall's weakest point. Inguinal hernias may contain abdominal organs (the small and large intestine, omentum, or bladder). Inguinal hernias are of two types: direct and indirect.
Indirect Inguinal Hernia
Indirect inguinal hernias emerge from the lateral edge of the inferior epigastric artery, exit through the deep inguinal ring, and pass through the inguinal canal. Therefore, when it becomes large enough, it can descend in men to the scrotum along the structures that go to the testis and in women to the labia majora. On the other hand, direct inguinal hernias do not descend into the scrotum because they are not located within the inguinal canal.
In males, indirect hernias follow the same route as the processus vaginalis (the descending testes). Therefore, indirect inguinal hernias have an embryological (congenital) origin. If there is a large opening in the processus vaginalis, an indirect inguinal hernia develops, and if there is a small opening, a hydrocele develops.
Indirect inguinal hernias are the most common type of hernia in both men and women. Inguinal hernias are 5–10 times more common in males than females. Indirect hernias are five times more common than direct hernias, and they carry a higher risk of incarceration.
Almost all pediatric inguinal hernias are indirect, and 75% are on the right. In the presence of a hernia on the left, it is likely to be bilateral. Therefore, after the left side is operated on, the right side is explored in the same session. The hernia type in patients with an undescended testicle (testis) or hydrocele is indirect.
Due to the incomplete closure of the processus vaginalis, an indirect hernia may be observed concomitantly with undescended testicles. If a sac is discovered during orchidopexy (the downward movement and repositioning of the testis), high ligation should always be performed.
Direct Inguinal Hernia
Direct hernias are acquired (secondary) due to muscle weakness, and they are more common in men. Direct inguinal hernias arise medially to the inguinal canal and inferior epigastric artery. In other words, direct inguinal hernias arise from the Hasselbach triangle and protrude directly from the superficial inguinal ring, bypassing the inguinal canal.
The boundaries of the Hasselbach triangle are;
- Lateral border: inferior epigastric vessels
- Medial border: rectus abdominis muscle
- Inferior border: inguinal ligament
Femoral Hernias
Femoral hernias develop from the femoral canal and occur in the anteromedial thigh. The femoral canal is located on the medial side of the femoral sheath, which surrounds the femoral vein, artery, and nerve. Because the femoral canal is narrow and not expandable, the hernia sac is easily strangulated. The medial-to-lateral arrangement of the structures in the femoral sheath are: veins, arteries, and nerves (VAN).
Femoral hernias occur in middle and old age (acquired). Since the pelvis is wider in females, femoral hernias are proportionally more common, but inguinal hernias are still the most common hernias in females.
Umbilical Hernias
Umbilical hernias are less common than inguinal hernias. Umbilical hernias are typically congenital and result from an incomplete closure of the umbilicus. The umbilicus is a weak point of the abdominal wall through which the umbilical cord passes. The majority of these hernias close within the first year of life without the need for surgery.
Incisional Hernias
Incisional hernias protrude through a defect in the scar tissue at the abdominal incision. If the neck of the hernia sac is wide, the probability of strangulation is low; if it is narrow, the probability of strangulation is high.
5. Encyclopedia of the Inguinal Region
Structures Originating from the Superficial Fascias (Camper and Scarpa)
- Camper's Fascia: It is also called subcutaneous fatty tissue. It is thinner in the upper abdomen and thicker in the lower abdomen. It is the superficial layer of the superficial fascia.
- Scarpa's Fascia: It is membranous and contains little or no fat. It begins below the navel and extends into the thigh. It is the deep layer of the superficial fascia.
- Buck's Fascia: It is an extension of Scarpa's fascia, the deep fascia of the penis, enveloping all three erectile bodies (the corpus spongiosum pair and the corpus cavernosum).
- Tunica Dartos: It is an extension of Scarpa's fascia, the fascia under the skin of the scrotum that continues as the superficial fascia of the penis.
- Colles' Fascia: It is an extension of Scarpa's fascia, the superficial fascia of the perineum.
Structures Originating from the External Oblique Muscle Aponeurosis
- Inguinal Ligament (Poupart’s Ligament): The inguinal ligament is the thickened lower edge of the external oblique muscle aponeurosis. It runs from the ASIS (anterior superior iliac spine) to the superior ramus of the pubis. The medial third is free. The lateral two thirds are attached to the iliopsoas muscle aponeurosis. In sutured hernia repairs such as Bassini, the sutures pass through the inguinal ligament. In tension-free hernia surgeries, the lower edge of the mesh is sutured to the inguinal ligament.
- Lacunar Ligament (Gimbernat’s Ligament): The lacunar ligament has the shape of a narrow isosceles triangle. It originates from the medial portion of the inguinal ligament and connects to the pectineal ligament (next to the pubic tubercle). It is approximately 1.25 cm long. The lacunar ligament forms the medial border of the vascular lacuna (lacuna vasorum), where the femoral artery and vein pass.
Reflected Ligament (Ligamentum Reflexum, Colles' Ligament, Fascia Triangularis Abdominis, Triangular Fascia)
The reflected ligament is a slightly strengthened portion of the external oblique aponeurosis. The reflected ligament is derived from the medial portion of the inguinal ligament and connects to the linea alba.
Pectineal Ligament (Cooper's Ligament)
The pectineal ligament is an extension of the lacunar ligament. It is a strong, thick ligament that is attached to the pectineal line on the pubic bone.
Femoral hernias can be repaired through Cooper ligament repair (McVay repair). In this technique, the conjoined tendon is sutured to Cooper's ligament. As a result, the entire myopectineal orifice, including the femoral canal (where the femoral hernia originates), is closed.
Conjoint Tendon (Henle’s Ligament, Inguinal Falx, Inguinal Aponeurotic Falx)
The conjoint tendon is the common aponeurosis of the internal oblique and transverse abdominal muscles. It attaches to the pubic crest and pectineal line of the pubis; it is often more muscular than an aponeurosis (95%). The conjoint tendon forms the medial third of the posterior wall of the inguinal canal.
The conjoint tendon is an important structure because, in most suture repairs, this area is sutured to another inguinal structure below. For example, in Bassini hernia repair, the conjoint tendon is sutured to the inguinal ligament (Poupart). In McVay repair, the conjoint tendon is sutured to the pectineal ligament (Cooper).
Interfoveolar Ligament (Hesselbach's Ligament)
The interfoveolar ligament starts from the lower border of the transverse muscle, medial to the internal ring, and attaches to the superior pubic ramus. Hesselbac’s ligament may be muscular or fibrous in nature.
Iliopubic Tract
The iliopubic tract is the thickened lower border of the fascia transversalis. It runs parallel to the inguinal ligament but is deeper. The iliopubic tract contributes to the posterior wall of the inguinal canal. It is easily seen in the posterior view of the abdominal wall in laparoscopic surgeries.
Spermatic Cord Contents (Structures)
Ductus Deferens (Vas Deferens)
The ductus deferens is the secretory duct of the testis. The testis empties its secretion into the epididymis. The extension of the epididymis is the ductus deferens. The vas deferens enters the abdomen through the inguinal canal. It joins with the seminal vesicle's ejaculatory duct and opens into the prostatic urethra.
Pampiniform Plexus
The pampiniform plexus is a network (plexus) formed by the veins of the testis and epididymis. It starts as 8–10 veins, falls into 3–4 veins in the inguinal canal, and decreases to 2 veins when it enters the abdomen. It then becomes a single vein and is called the testicular vein (internal spermatic vein). On the right, the testicular vein empties into the inferior vena cava, and on the left, it empties into the left renal vein.
The pampiniform plexus is a spermatic cord structure that is located in the inguinal canal in front of the ductus deferens. This plexus is also part of the system that regulates the temperature of the testes. Thus, the testicular temperature is kept slightly lower than the body temperature. Its abnormal (varicose) dilatation is called a varicocele. Incompetent valves in the testicular vein (internal spermatic vein or gonadal vein) cause varicocele.
In females, the pampiniform plexus is formed by the ovarian veins. It is located in the broad ligament of the uterus (ligamentum latum uteri).
Gonadal Arteries
In men, the testicular arteries (also called the internal spermatic artery) are gonadal arteries. In women, the ovarian arteries are gonadal arteries. Gonadal arteries are paired arteries that originate from the abdominal aorta.
Testicular Arteries
Testicular arteries are long, thin pairs of arteries that arise from the aorta just below the renal arteries and go to the testicles. It is a structure of the spermatic cord. It supplies the testis, epididymis, cremasteric muscle, and the lower part of the ureter.
Ovarian Arteries
Ovarian arteries originate from the aorta just below the renal arteries, and they supply the ovaries. The ovarian arteries emerge from the aorta and run through the suspensory ligament of the ovary before entering the mesovarium. The ovarian artery can anastomose with the uterine artery in the ligamentum latum uteri (broad lig).
The ovarian arteries are the equivalent of the testicular arteries, but they are shorter. The origin of both arteries is the same, but at the level of the lesser pelvis, the ovarian arteries are directed into the abdomen and go to the ovaries. So the ovarian arteries are not a structure of the spermatic cord. The testicular arteries, on the other hand, exit the abdomen by passing through the internal (deep) inguinal ring, run as a cord structure in the inguinal canal, and go to the testes.
Arcuate Line (Semicircular Line (of Douglas))
The horizontally curved arcuate line forms the lower border of the rectus sheath's posterior layer. The arcuate line is about halfway between the umbilicus and the pubic crest. In other words, the posterior sheath of the rectus muscle is absent below the arcuate line, and the rectus muscle is in contact with the transversalis fascia. The inferior epigastric arteries enter the rectus muscle near the arcuate line. Spigelian hernias occur at the Spigelian line, which is below the arcuate line, or where the Spigelian line and the arcuate line meet.
Semilunar Line (Spigelian Line), Spigelian Fascia and Spigelian Hernia
There are two main definitions of linea semilunaris:
- The semilunar line is the muscle-fascia border (junction) of the transverse abdominal muscle. In other words, it corresponds to the medial border of the transverse abdominal muscle.
- The semilunar line refers to the lateral edge (border) of the rectus abdominis muscles
The semilunar line extends from the 9th rib to the pubis. It's about halfway between the lateral edge of the trunk and the median line, and a few centimeters medial to the midclavicular line. When the rectus muscles are stretched, the semilunar line appears as a groove on the rectus abdominis muscle edges.
There are two main definitions of Spigelian fascia (aponeurosis):
- Spigelian fascia (maybe more precisely Spigelian zone) is the aponeurotic layer between the rectus abdominis muscle medially and the semilunar line laterally (medial border of the transverse abdominal muscle). Spigelian fascia refers to the intersection of the aponeuroses of the 3 lateral abdominal wall muscles along the lateral border of each rectus abdominis muscle (Skandalakis):
- External oblique muscle aponeurosis (fuses with the anterior leaf of the internal oblique muscle aponeurosis to form the anterior rectus sheath)
- Anterior and posterior leaf of the internal oblique muscle aponeurosis,
- Transversus abdominis muscle aponeurosis (fuses with the posterior leaf of the internal oblique muscle aponeurosis to form the posterior rectus sheath)
- Spigelian aponeurosis (fascia) is comprised of the transversus abdominis and internal oblique aponeurosis, bounded by the linea semilunaris laterally (medial border of the transversus abdominis muscle) and the lateral edge of the rectus muscle medially (UpToDate).
Spigelian hernias are caused by a defect in the Spigelian fascia; however, they are covered by an intact external oblique aponeurosis. Because the hernia sac is located between the layers of the anterior abdominal wall and not under the skin, Spigelian hernias are called interparietal (intraparietal, interstitial) hernias. Spigelian hernias can occur anywhere in the Spigelian zone, but they occur most often near the arcuate line.