Breast - Overview
- Overview
- Breast in Menopause
- Male Breast
- Congenital and Developmental Abnormalities of the Breast
- Mastalgia (Breast Pain)
- Ductal Ectasia of Breast
- Fibrocystic Breast Changes
- Periductal Mastitis (Zuska’s Disease)
- Sclerosing Adenosis of the Breast
- Radial Scar of the Breast
- Mastitis
- Mondor's Disease
- Breast Cancer
- Where Does Breast Cancer Start in the Breast?
- Proto-Oncogenes
- Tumor Suppressor Genes
- Inherited Gene Alterations
- Acquired Gene Alterations
- Breast Cancer Rates in terms of Genetic Transmission
- How does breast cancer spread?
- Frequency of Breast Cancer
- Prognosis and Survival of Breast Cancer
- Symptoms of Breast Cancer
- Treatment of Breast Cancer
1. Overview
Bacteremia. Breasts are a disadvantage for women in terms of breast diseases. Women are 100 times more likely to have breast cancer than men. Breast cancer is the most common type of cancer in women worldwide, particularly those over the age of 50 (menopause). The 5-year survival rate is 100% if caught early (Stage 1), 93% in Stage 2, 72% in Stage 3, and 22% in Stage 4.
Although the majority of breast lesions are palpable and benign, they can all be confused with breast cancer. This is especially important in fibrocystic changes, which are the most common cause of breast masses.
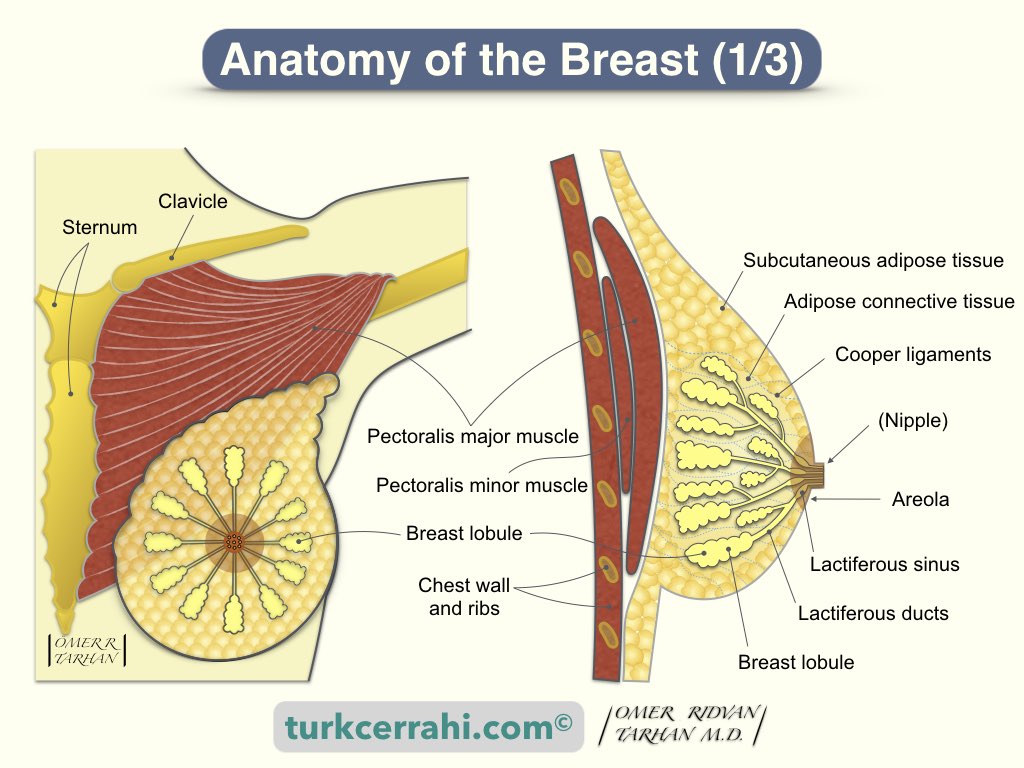
The breast is a glandular organ located on the chest. The breast is made up of connective tissue, fat, and breast tissue that contains the milk-producing glands.
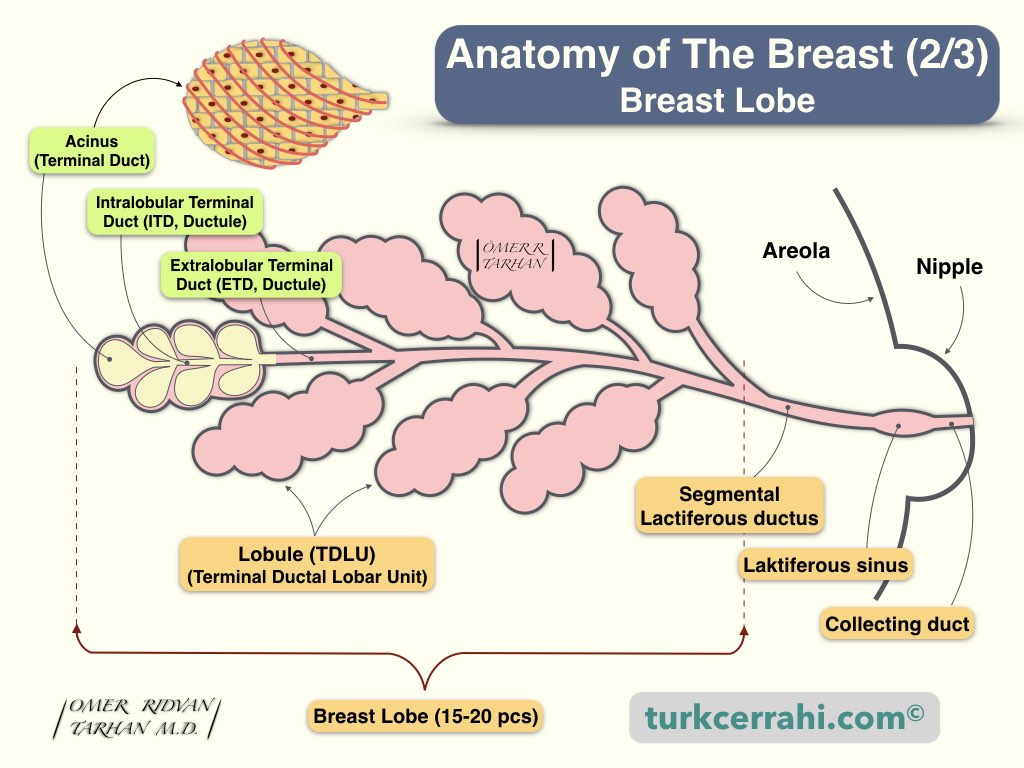
Breasts are skin glands (apocrine glands) of ectodermal origin. The breast in women who have not given birth has not fully matured. Ductal (lactiferous duct) epithelium is more common, and alveolar (mammary gland) epithelium is less common. During pregnancy, the breast is prepared to give milk. Ductal, lobular, and alveolar (milk gland) development occurs.
2. Breast in Menopause
Glandular tissue in the breast decreases in menopause. It is replaced by adipose tissue (fat). Postmenopausal breast tissue consists of abundant adipose tissue, connective tissue, and lactiferous ducts. When fatty tissue in the breasts is reduced, the breasts become ptotic.
3. Male Breast
Before puberty, the development of the male breast is similar to that of the female breast. Estrogen and progesterone levels do not rise after puberty, and male breasts (lobules) do not develop. The male breast is rudimentary (underdeveloped) and consists of only small ducts. Therefore, breast cancer that develops in men is called ductal carcinoma. Lobular breast cancer is almost never seen.
4. Congenital and Developmental Abnormalities of the Breast
- Amastia: Absence of breast tissue and nipple-areola complex.
- Amazia: Absence of breast tissue, but the nipple and areola are present.
- Athelia: Absence of nipple-areola complex, but the breast tissue is present.
- Breast Hypoplasia: Mammary hypoplasia, underdeveloped breasts, insufficient glandular tissue (IGT), tubular breasts. The breasts may be small, normal, or large, but the mammary tissue did not develop properly during adolescence, which can cause low or no milk production. Breast hypoplasia can be unilateral or bilateral. Spaced breasts, asymmetries, and the absence of breast changes during pregnancy and the postpartum period are signs of breast hypoplasia.
- Micromastia: Also called hypomastia, breast aplasia, small breasts: Breasts remain small after puberty.
- Symmastia (breasts fused to the midline): Symmastia is the union of both breasts in the midline (presternal region). The skin is elevated in the midline, and the depth of the intermammary sulcus (cleft) is reduced or completely disappeared. Symmastia is rarely congenital, more often, occurs with oversized, poorly positioned, or displaced implants (to the middle).
- Polymastia: It is the presence of accessory (ectopic, out of place) breasts along the milk line.
- Polythelia: Accessory nipple, presence of more than one (multiple) nipple).
- Accessory Axillary Breast: Breast tissue continues towards the axilla on both sides.
- Gynecomastia In Men (Big Breasts): It is an enlargement of the mammary gland in boys and men. Pseudo gynecomastia or lipomastia, which is characterized by an increase in adipose tissue without enlarging the mammary gland, is a different situation. Gynecomastia can be unilateral or bilateral and treated by liposuction or surgery (subcutaneous mastectomy).
5. Mastalgia (Breast Pain)
Mastalgia is pain originating from breast tissue.
Mastalgia Types
- Periodic Mastalgia (Cyclic Mastalgia)
- Non-Cyclic Mastalgia
Periodic Mastalgia (Cyclic Mastalgia)
It is very common among women of childbearing age. It starts 5-7 days before the menstrual period and lasts for an average of 1-4 days. Pain often ends with menstruation.
Non-Cyclic Mastalgia
There is no relation to the menstrual period. Non-cyclic mastalgia occurs at any menstrual cycle phase and is more common in women over the age of 40 and in menopausal women. It is generally described as burning, pulling, tingling, and throbbing in the breast. Causes of non-cyclic breast pain include pregnancy, mastitis (breast infection), trauma, macrocysts, benign tumors, and cancer. For this reason, it is important to consult a doctor.
Treatment of Mastalgia
If the cause of breast pain is an abscess, an infection, or any other pathology, the underlying disease is treated. No special treatment is necessary if the pain is associated with the menstrual cycle and does not cause serious complaints; pain relievers are sufficient.
Applying hot or cold compresses to the chest, wearing a bra that is appropriate for the body and provides tight support, wearing a sports bra while exercising and sleeping, reducing the fat ratio in meals, limiting or eliminating caffeine consumption, and using pain relievers can all help alleviate breast pain.
6. Ductal Ectasia of Breast
Ductal ectasia of the breast is the enlargement and thickening of the milk ducts beneath the nipple. Enlarged ducts are filled with fluid. It is generally seen in the perimenopausal period (45–55 years) and causes a dirty yellow, green, or black discharge from the nipple. Ductal ectasia can lead to periductal mastitis, which makes the nipple and tissue around it red and tender, and nipple retraction.
Ductal Ectasia Treatment
Ductal ectasia does not always require treatment and may improve on its own. Hot packs or antibiotics may be used to treat periductal mastitis. They are rarely removed surgically.
7. Fibrocystic Breast Changes
Fibrocystic breast changes are benign conditions characterized by cysts, masses, pain, and tenderness in the breasts. Symptoms generally worsen before menstruation. Fibrocystic breast changes do not cause or transform into breast cancer. But fibrocystic breast changes can make the diagnosis of breast cancer difficult and may be confused with cancerous masses.
Just like in the uterus, the mammary glands are prepared for pregnancy from the beginning of the menstrual period (with the effect of estrogen and progesterone hormones). During these cyclic changes, which are also seen in the milk ducts, fibrosis develops in the milk ducts of some women’s breasts over time.
Even though the mammary glands do not produce milk, they can maintain their secretion. Normally, secreted fluid is reabsorbed in the milk ducts. This fluid cannot be reabsorbed when milk ducts and glands are damaged due to fibrocystic changes. Or, sometimes fluid secretion increases excessively and fluid-filled sacs develop, called cysts. Breast cysts can be microscopic or large macrocysts, 6-7 cm in diameter.
Fibrocystic changes are more common after the age of 30 because the fibrotic events described above are repeated for years, resulting in permanent changes. After the age of 50, when menopause begins, fibrocystic changes stop.
Treatment of Fibrocystic Breast Changes
- Reducing the Complaints (Symptomatic Treatment): First of all, painkillers and anti-inflammatory drugs can be used for complaints such as burning pain. Wearing a bra suitable for the breast also provides relief.
- Correction of Hormonal Disorders, if any: Irregular menstruation increases the patient's breast complaints. It is suggested that the regulation of menstrual disorders with birth control pills (oral contraceptives) in these patients is beneficial.
- Lifestyle and Dietary Changes: Caffeine has been reported to increase fibrocystic changes. Food and drinks with caffeine such as coffee, tea, cola drinks, and chocolate should be limited. Fermented foods such as beer, cheese, and wine should also be limited.
8. Periductal Mastitis (Zuska’s Disease)
Periductal mastitis develops due to chronic inflammation of the subareolar ducts. Most patients with periductal mastitis are young female smokers. It is usually seen between the ages of 30 and 40. Smoking is the most important risk factor for periductal mastitis.
Squamous metaplasia of the lactiferous ducts (SMOLD) results in subareolar milk duct occlusion and obstruction, recurrent subareolar abscesses (periductal mastitis), and periductal fistulas.
Initial treatment for periductal mastitis and subareolar abscesses, respectively, is antibiotic therapy and abscess drainage. If it recurs, subareolar exploration is required (total duct excision; cylindrical excision of breast tissue containing the milk ducts behind the areola.)
9. Sclerosing Adenosis of the Breast
Sclerosing adenosis is one of the benign proliferative diseases of the breast. The number of acini (an epithelial structure) per terminal duct has increased. The normal acini structure has changed, and the myoepithelial cell has become dominant. Sclerosing adenosis can cause multiple, small, hard and soft fibrous tissue nodules in the breast.
The treatment of sclerosing adenosis of the breast is excision. Despite the fact that sclerosing adenosis is not a precancerous lesion, it is associated with an increased risk of developing breast cancer. Studies have shown that women with sclerosing adenosis have a 1.5- to 2-times higher risk for breast cancer.
10. Radial Scar of the Breast
A radial scar, or complex sclerosing lesion, is an idiopathic proliferative breast lesion.
Breast examination, including radial scar areas, is usually normal. The radial scar is palpable in only 25% of cases and does not cause skin thickening or retraction.
Lesions are typically small, and mammography detects them when they are larger than 5 mm in size. When the lesions are smaller than 1 cm, they are called radial scars, and when they are larger than 1 cm, they are called complex radial sclerosing lesions.
A biopsy is required for differential diagnosis because a radial scar can be confused with cancer.
11. Mastitis
Mastitis is an inflammation of the breast, usually caused by a bacterial infection. It is most common in breastfeeding mothers, but it can affect any woman. A clogged milk duct that may cause bacterial overgrowth or cracks in the nipple may be an entrance for bacteria. Breast infection and inflammation cause edema (swelling and hardening), erythema (redness), and tenderness. Yellow, green, or brown discharge is common on the nipple. Patients may also have a fever, headache, or other general flu-like symptoms.
Diagnosis of Mastitis
Mastitis is typically diagnosed based on symptoms and a physical examination of the breasts. It usually affects only one breast.
Treatment of Mastitis
Mastitis is typically treated with antibiotics. A 10-day antibiotic therapy (penicillin, cephalosporin group) is administered. Breastfeeding should never be interrupted. The breast should be emptied even if breastfeeding is discontinued. Milk accumulating inside worsens infections and abscesses.
If there is no improvement after 48 hours of treatment, the patient should be evaluated for an abscess, and if an abscess is present, drainage should be performed.
If there is no improvement after one week of long-term antibiotic treatment, inflammatory breast cancer should be considered, and a skin biopsy should be performed to confirm the presence of cancer. Inflammatory breast cancer has symptoms very similar to mastitis.
How does mastitis affect the risk of breast cancer?
Mastitis does not increase the risk of developing breast cancer.
12. Mondor's Disease
Mondor's disease is thrombophlebitis of the superficial veins of the chest wall, also called superficial thrombophlebitis of the breast. It can affect any of the vessels in the breast, but most often it affects the vessels in the anterolateral breast. The disease was first described in 1939 by French surgeon Henri Mondor (1885–1962).
Symptoms of Mondor's Disease
When the arm on the affected side is raised, a shallow retraction (groove) is seen in the breast. The thrombosed vein is palpated as a thick, tender, painful, and red cord.
Diagnosis of Mondor's Disease
A clinical diagnosis can be made by taking a detailed medical history and performing a complete physical examination. A biopsy is rarely necessary for diagnosis. The absence of blood flow in the superficial veins of the breast on Doppler USG indicates Mondor's disease. On mammography, the vessels may appear dilated and tubular.
Treatment of Mondor's Disease
Mondor's disease usually resolves spontaneously within 4-6 weeks. However, some conservative treatment modalities can be used. Warm compresses can be applied. Nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, ibuprofen, and indomethacin, relieve symptoms (pain). NSAIDs can be taken orally or topically (as a gel). It is helpful to wear a supportive bra.
13. Breast Cancer
Cancer begins with uncontrolled cell division and proliferation. Normal cells divide as needed and die when their task is completed. Over time, cancer cells spread both to where they started (invasion) and to distant organs (metastasize), replacing normal cells and invading them. Cancer can start anywhere in the body.
Cancer is not a single disease. Cancer can start in the lungs, breasts, large intestine, or even in the blood. The growth and spread of cancers are different from each other.
Breast cancer begins with the uncontrolled proliferation of cells in the breast. Breast cancer cells proliferate and form a palpable mass (tumor or lump). These masses can be seen on X-rays (mammography). Cancer cells can invade surrounding tissues (e.g., chest wall, breast skin) or spread to distant parts of the body (metastasize: bones 70% (mostly vertebra), brain 10%, liver 10%, lung 10%).
The spread of cancer cells is called metastasis. If breast cancer spreads to the bones, it is still called breast cancer (metastatic breast cancer). Cancer cells in the bones are also similar to breast cancer cells. If cancer has not started in the bones, it is not called bone cancer.
Where Does Breast Cancer Start in the Breast?
The breast consists of 3 main structures
- Mammary gland (mammary gland= alveoli (acini) + ducts (milk ducts))
- Fatty connective tissue
- The skin of the breast
Breast cancer mainly originates from two structures:
- The milk ducts (ductal carcinoma, 90% of cases) and
- The lobules (milk producing part, lobular carcinoma, 10% of cases).
Rarely, cancer may develop in other tissues in the breast. These cancers are called sarcomas and lymphomas and are not considered true breast cancers.
Why and How Does Breast Cancer Start?
Due to pre-existing (inherited) or new (de novo) DNA mutations, breast cells can mutate into cancer cells.
Inherited DNA changes from your parents significantly increase your risk of breast cancer. Environmental factors (food, estrogen, obesity, not doing sports, etc.) cause mutations in breast cells (DNA deterioration), causing them to become cancer cells.
Some genes control the division, development, and death of our cells. Changes in these genes cause the development of cancer.
Proto-Oncogenes
Proto-oncogenes are genes that help cells grow normally. If a proto-oncogene mutates (changes, degenerates) or increases in number, it means that it has become a hazardous "oncogene" (oncogene = cancer-causing gene). Even when there is no need for cell division in a tissue, the oncogene encourages cells to divide and grow, and cancer occurs. Let's explain: the proto-oncogene is like the gas pedal of a car. The car is accelerated when needed.
An oncogene is like a stuck gas pedal; the control is gone.
Tumor Suppressor Genes
Tumor suppressor genes are normal genes. It slows cell division, repairs DNA errors, and tells cells when to die (apoptosis: programmed cell death). If tumor suppressor genes don't work properly, cells grow out of control, multiply, and don't die when they should. This causes cancer.
A tumor suppressor gene is like a brake pedal.
Inherited Gene Alterations
Certain inherited DNA mutations (changes, alterations) can significantly increase the risk of developing certain cancers and are linked to some cancers that run in some families. For example, the BRCA genes (BRCA1 and BRCA2) are tumor suppressor genes. When one of these genes is changed, it no longer suppresses abnormal cell growth, and cancer is more likely to develop. Changes in these genes can be passed on from parent to child.
Acquired Gene Alterations
A new mutation may develop in oncogenes and/or tumor suppressor genes (de novo mutation). Environmental factors contribute to the development of new gene mutations, but the precise causes of acquired mutations are unknown.
The use of biomarkers ensures that breast cancer patients receive optimal treatment. These tests also provide information about the prognosis. For example, breast cancers with high levels of the HER2 oncogene grow and spread (metastasize) more quickly. A benefit of the test is the availability and administration of drugs that target HER2-positive cancer cells. In other words, HER2-targeted therapies improve survival outcomes significantly in patients with HER2-positive breast cancer.
Breast Cancer Rates in terms of Genetic Transmission
- Sporadic breast cancer (65-70%)
- Familial breast cancer (20-30%)
- Hereditary breast cancer 5-10%
- BRCA-1 (45%)
- BRCA-2 (35%)
How does breast cancer spread?
Breast cancer can spread (transport to other parts of the body) when cancer cells enter the blood or lymph system. Breast cancer first spreads to the lymph nodes and then jumps to the blood and distant organs.
The lymphatic system is a network of vessels that carries the lymph fluid found throughout the body. Lymph nodes are small, bean-shaped structures located on lymphatic vessels. Lymph nodes are part of the immune system and contain T and B lymphocytes. The lymph nodes filter bacteria, foreign bodies, and cancer cells.
Lymphatic vessels transport lymphatic fluid from the breast to the systemic circulation (blood vessels). Breast cancer cells may enter these lymph vessels and begin to multiply in the lymph nodes. Metastatic lymph nodes are large, firm, and have irregular borders. Certain areas have more lymph vessels and thus more lymph nodes.
- Lymph nodes in the armpit (axillary lymph nodes)
- Lymph nodes above and below the collarbone (supraclavicular and infraclavicular lymph nodes)
- Lymph nodes at the edge of the breastbone (sternum), (internal mammary lymph nodes)
Breast cancer cells can spread to distant organs via blood circulation following lymph node involvement (distant metastasis). Bone, brain, liver, and lung are the most common.
Frequency of Breast Cancer
Except for skin cancer, breast cancer is the most common cancer in women worldwide. The average risk for a woman to develop breast cancer at some point during her life is around 12% (1/8).
Prognosis and Survival of Breast Cancer
Natural Course of Breast Cancer (In Untreated Patients)
Over time, cancer in the breast grows, invades the skin of the breast, and causes a large ulcer on the skin (75%). This ulcer does not result in the patient's death. Metastasis to the lung, liver, bone (especially the vertebra), and brain is the primary cause of breast cancer mortality (death of the patient).
5-Year Survival in Breast Cancer Untreated Patients
According to a study of 250 patients, the average survival of untreated breast cancer patients is 2.7 years. 5-year survival (life) is 18%, and 10-year survival (life) is 3.6%. 95% of untreated breast cancer patients die from breast cancer and 5% from other causes.
5-Year Survival in Patients Treated for Breast Cancer
Generally, five-year survival rates are given. 5-year survival is the proportion of patients who have lived at least 5 years after diagnosis. The 5-year survival rates for stages 1, 2, 3, and 4 are 100%, 93%, 72%, and 22%, respectively.
Symptoms of Breast Cancer
- Hard mass in the breast (usually ductal carcinoma)
- Enlargement of the entire breast (usually lobular carcinoma)
- Edema of the breast and breast skin (edema causes an orange peel appearance, peau d'orange)
- Breast pain, and redness (rare, seen in inflammatory breast cancer)
- Retracted nipple (nipple is pulled inward)
- Dimpling on the breast skin
- Masses in the axilla (armpit) (metastatic lymph nodes)
- Bloody discharge from the nipple (intraductal carcinoma)
Knowing how your breasts normally look and performing a self-exam are important parts of breast health. Mammography scans allow the diagnosis of breast cancer before symptoms appear. Early diagnosis increases the success of treatment.
Breast Mass
The most common symptom of breast cancer is the appearance of a new mass in the breast that did not exist before. In breast cancer, the mass is firm (hard), painless, and has irregular borders. Exceptions: In lobular carcinoma, the entire breast is enlarged, and usually no mass forms; in inflammatory breast cancer, the mass is painful, and there is redness and edema in the breast. Symptoms may vary according to the pathological type of cancer.
Treatment of Breast Cancer
Breast cancer patients may receive one or more of the following treatments, depending on the stage of their disease:
- Local Treatments in Breast Cancer
- Surgical
- Radiotherapy
- Systemic Treatments in Breast Cancer
- Chemotherapy
- Hormone therapy (hormone therapy)
- Targeted therapy