Anatomy of the Breast
- Introduction
- Functional Anatomy of the Breast
- The Suspensory Ligaments of Cooper (Suspensory Ligament of Breast)
- Nipple and Areola (Nipple - Areola Complex)
- Milk Line (Mammary Ridge)
- Arteries of the Breast
- Veins of the Breast
- Innervation of the Breast
- Lymphatic Drainage of the Breast
- Anatomy of the Axilla
- Breast in Menstruation
- Breast in Pregnancy
- Breast in the Lactation Period
- Breast in Menopause
- Male Breast
1. Introduction
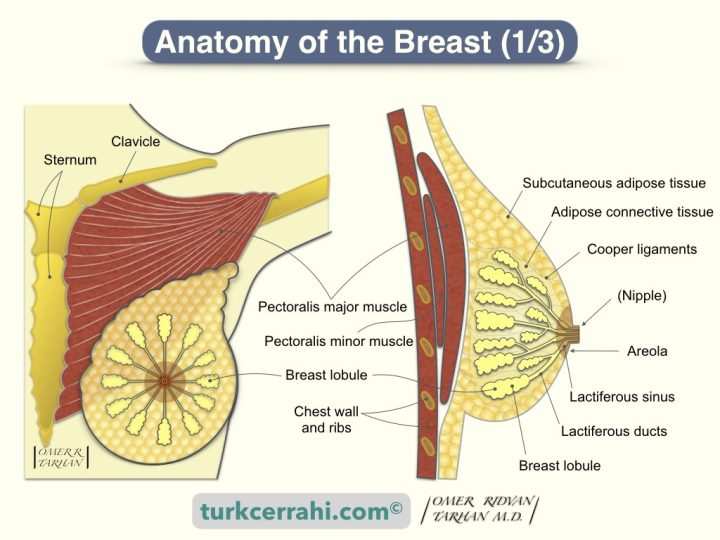
Adult female breasts of various sizes are located on the anterior thoracic wall, between the second and sixth ribs inferiorly and superiorly, the sternum medially, and the anterior axillary line laterally. The breast is 10-12 cm in diameter and attached to the major pectoral muscle posteriorly.
The upper outer part of the breast extends into the axilla (axillary tail of Spence, axillary process). The position of the nipple and areola varies according to the size of the breast.
2. Functional Anatomy of the Breast
The breast consists of mammary glands, connective tissue, and overlying skin.
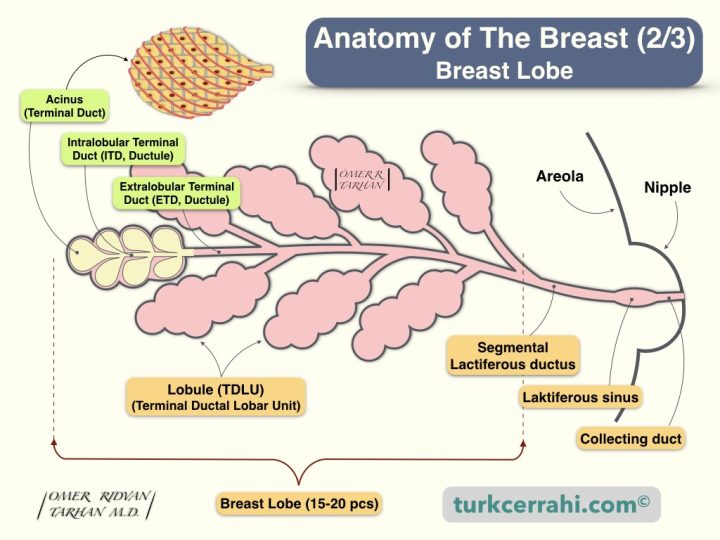
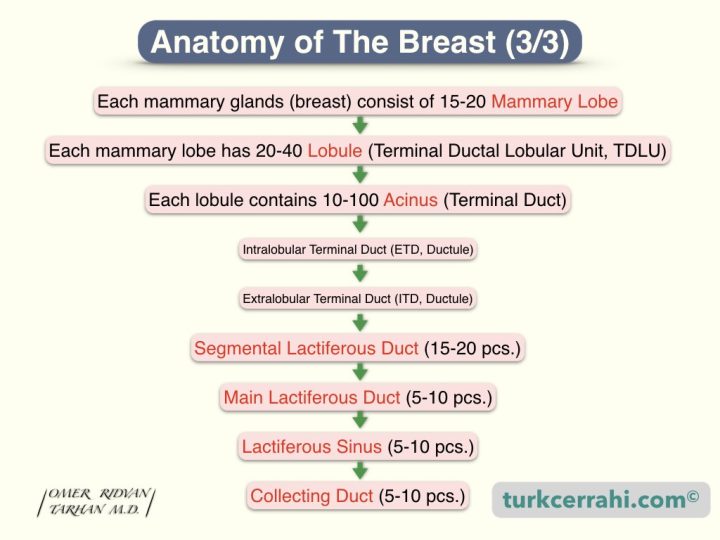
- The mammary glands (breast) consist of 15-20 mammary lobes.
- Each mammary lobe has 20-40 Lobules (Terminal Ductal Lobular Unit, TDLU)
- Each lobule contains 10-100 acinus (Terminal Duct)
- Intralobular terminal duct (ETD, Ductule)
- Extralobular terminal duct (ITD, Ductule)
- Segmental lactiferous ducts (15-20 pcs.) (Single-layered cuboidal epithelium)
- Main lactiferous ducts (5-10 pcs.) (Bi-layered cubic epithelium)
- Lactiferous sinus (5-10 pcs.) (Multi-layered squamous epithelium)
- Collecting ducts (5-10 pcs.)
3. The Suspensory Ligaments of Cooper (Suspensory Ligament of Breast)
The Suspensory Ligaments of Cooper are formed by thickening some parts of the connective tissue network that gives the breast its shape. One end of the Cooper ligament adheres to the breast skin and disperses, and the other end adheres to the chest wall and clavicle. In breast cancer, the Cooper ligaments of the breast are stretched or shortened and cause retraction in the breast skin (dimpling). (Astley Cooper 1768-1841, English surgeon, anatomist)
Cooper's ligament of the breast should not be confused with the pectineal ligament (Cooper's inguinal ligament). In addition, the ulnar collateral ligament is sometimes called Cooper's ligament.
4. Nipple and Areola (Nipple - Areola Complex)
The areola and the nipple are pigmented (darker) and rough. During pregnancy, the breast and nipple become darker, and the nipple enlarges.
The areola contains the sebaceous and sweat glands and the Montgomery tubercles (small bumps). Circular smooth muscle fibers of the areola and nipple are responsible for nipple erection.
5. Milk Line (Mammary Ridge)
The milk line is a thickened ectoderm line that begins to develop in the 5th-6th weeks of the embryo and extends from the axilla to the inguinal region in the front of the trunk of both sexes.
The breast and nipple develop along this line. These lines disappear after a short time. Accessory breasts (polymastia) or accessory nipples (polythelia) develop on this line.
6. Arteries of the Breast
Laterally
- Axillary artery
- Superior thoracic artery
- Thoracoacromial artery
- Lateral thoracic artery
- Subscapular artery
Medially
- Branches of internal thoracic artery
Posteriorly
- Perforating arteries from II to IV intercostal arteries
7. Veins of the Breast
The veins in the breast run parallel to the arteries and drain into the axillary vein, the internal thoracic veins, and the anterior intercostal veins.
8. Innervation of the Breast
- The intercostal nerves from II to VI
- Nipple, intercostal nerve IV
9. Lymphatic Drainage of the Breast
- 75% of the lymphatic drainage of the breast drains into the axillary lymph nodes (Schwartz 8th edition)
- Axillary lymph nodes are embedded in the adipose tissue here (axillary fat pad).
- Most of the remaining lymphatic fluid drains into the lymph nodes around the internal thoracic artery (parasternal lymph nodes, internal mammary lymph nodes).
- Surgeons call the internal thoracic artery the internal mammarian artery.
- The superior epigastric artery is the continuation of the internal thoracic (mammary) artery.
- Rotter lymph nodes are the lymph nodes between the pectoralis major and minor muscles.
Axillary Lymph Nodes
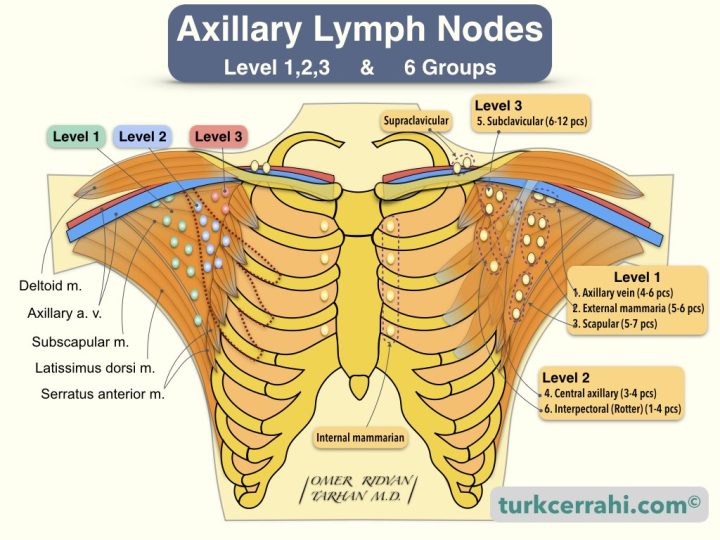
Surgeons Define 6 Groups of Lymph Nodes
- Axillary vein group (4-6 lymph nodes)
- External mammarian group (anterior, pectoral group) (5-6 lymph nodes)
- Scapular group (posterior, subscapular) (5-7 lymph nodes)
- The central group (3-4 lymph nodes)
- Subclavicular group (apical) (6-12 lymph nodes)
- Interpectoral group (Rotter ganglion) (1-4 lymph nodes)
Axillary Lymph Nodes Related to Pectoralis Minor Muscle
- Level I (1) Axillary Lymph Nodes (Lateral to the pectoralis minor muscle, groups 1,2,3)
- Axillary vein group
- External mammarian group
- Subscapular group
- Level II (2) Axillary Lymph Nodes (Behind the pectoralis minor muscle, groups 4-6)
- Central group
- Interpectoral group
- Level III (3) Axillary Lymph Nodes (5th group medial to the pectoralis minor muscle)
- Subclavicular group
10. Anatomy of the Axilla
Borders of Axilla
- Laterally; the latissimus dorsi muscle
- Superiorly; axillary vein
- Medially; the thoracic wall
- Inferiorly; the intersection of the serratus anterior muscle and the latissimus dorsi muscle
- Posteriorly (base); subscapularis muscle
Structures in the Axilla
- Axillary fat pad and lymph nodes inside it
- Intercostobrachial nerve: Sensory nerve on the medial surface of the arm
- Long thoracic nerve (Bell): It is the motor nerve of the serratus anterior and subscapularis muscles.
- Thoracodorsal nerve: It is the motor nerve of the latissimus dorsi muscle. The thoracodorsal nerve is found together with the thoracodorsal artery and vein.
11. Breast in Menstruation
For a woman who has not given birth, her breast development has not been completed. There is more duct epithelium and less alveolar epithelium.
Breast fullness and pain are minimal for 5–7 days after menstruation. As a result, the examination and detection of the breast and the mass in the breast are easiest during this period. Until the 14th day, proliferation (the estrogen effect) is seen in the breast epithelium, and after the 14th day, differentiation and secretion are seen in the dilated alveolar epithelium in the ducts (the progesterone effect). In the following days, the blood supply of the breast increases, and there is some edema in the breast. All of these together cause premenstrual growth, fullness, and tenderness in the breast. With the onset of menstruation, the levels of the hormones estrogen and progesterone fall precipitously, and the associated changes (involution) return. Breast nodularity in menstruating women is caused by varying amounts of proliferation and involution in each cycle and in different parts of the breast.
12. Breast in Pregnancy
- During pregnancy, the breast is prepared to give milk. Ductal, lobular and alveolar development occurs. It is due to the following hormones
- Estrogen
- Progesterone
- Placental lactogen
- Prolactin
- Chorionic gonadotropin.
- 1st trimester, early period
- Budding and lobular development in the ducts (estrogen
- 1st trimester, late period
- Breast enlargement
- Enlargement of the superficial veins
- Increased pigmentation of the nipple and areola
- 2nd trimester
- Lobule structure continues to develop (progesterone)
- Colostrum (first milk) accumulates in the alveoli
- 3rd trimester
- Breast size can triple.
13. Breast in the Lactation Period
- Placental lactogen and sex hormones (estrogen, progesterone) decrease with birth
- After that, pituitary-derived prolactin produces milk (from alveoli)
- Colostrum, also called foremilk (first 4-5 days)
- The protein content is richer than normal breast milk
- Contains plenty of antibodies, antibodies protect the baby from diseases
- It is a mild laxative, making it easier for the baby to make meconium.
- Concentrated (less amount, more nutritive)
- Breast milk
- Higher lipid content than colostrum
- Prolactin (anterior pituitary) and oxytocin (posterior pituitary) hormones provide the continuity of milk (lactation).
- Baby's suckling increases both of these hormones (tactile stimulation)
- An obstacle to milk discharge also facilitates the growth of bacteria (lactational mastitis). An infection in the areola causes obstruction of the milk ducts, which in turn causes mastitis.
- Post Lactational involution (return of the breasts after breastfeeding)
- Breasts regain their original shape within 3 months when breastfeeding is stopped.
- Glandular and ductal atrophy occurs, and the extralobular matrix regresses
14. Breast in Menopause
- Glandular tissue is reduced. Fat tissue takes its place.
- Postmenopausal breast tissue consists of abundant adipose tissue, connective tissue, and ducts.
- If the adipose tissue is low, the breasts become ptotic (sagging)
15. Male Breast
- Before puberty, the development of the male breast is similar to the female breast.
- Since estrogen and progesterone do not increase after puberty, male breasts (lobules) do not develop.
- The male breast is rudimentary (underdeveloped) and consists of only small ducts.
- Therefore, breast cancer that develops in men is ductal carcinoma. Lobular breast cancer is almost never seen.