Anatomy of the Colon
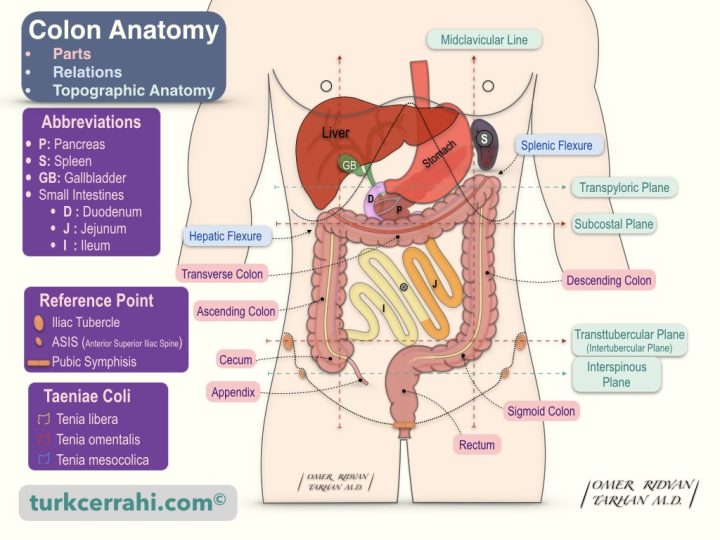
- Introduction
- Parts of the Large Intestine
- Difference Between Small and Large Intestine
- Peritoneal relations of colon and taeniae coli
- Cecum
- Appendix (Appendix Vermiformis)
- Ascending Colon
- Transverse Colon
- Descending Colon
- Sigmoid Colon
- Rectum
- Anal Canal
- Ligaments of the Colon
- Arteries of the Colon
- Veins of the Colon
- Lymph Vessels and Nodes of The Colon
- Nerves of the Colon
1. Introduction
The large intestine is the last part of the digestive system. Anatomically and functionally, the large intestine is divided into the colon, rectum, and anal canal.
The colon is a thicker tube than the small intestine, about 150 cm long, through which stool is formed and stored. The colon narrows distally. It is about 7.5 cm wide in the cecum and only 2.5 cm wide at the end of the sigmoid colon.
The liquid small intestine contents are poured into the colon, which absorbs the water and salt of this content and forms solid or semi-solid stool. Colon and rectal cancers are in 3rd place in men and 2nd place in women worldwide.
2. Parts of the Large Intestine

- Colon
- Cecum and Appendix
- Ascending colon
- Hepatic Flexure
- Transverse colon
- Splenic Flexure
- Descending Colon
- Sigmoid Colon
- Rectum
- Anal Canal
3. Difference Between Small and Large Intestine
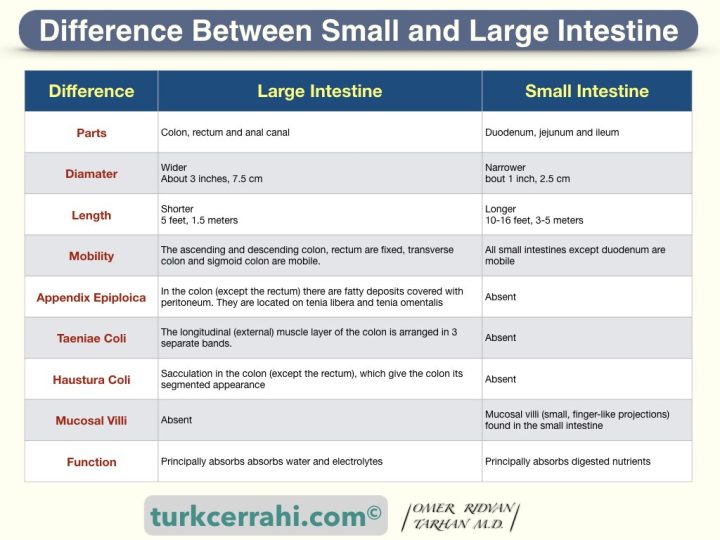
- Diameter: The diameter of the colon (about 3 inches, 7.5 cm) is larger than the small intestine (about 1 inch, 2.5 cm).
- Length: The small intestine is longer (about 10-16 feet, 3-5 meters) than the large intestine (about 5 feet, 1.5 meters).
- Appendix Epiploica: In the colon (except the rectum) there are fatty deposits covered with peritoneum. They are located on taenia libera and taenia omentalis.
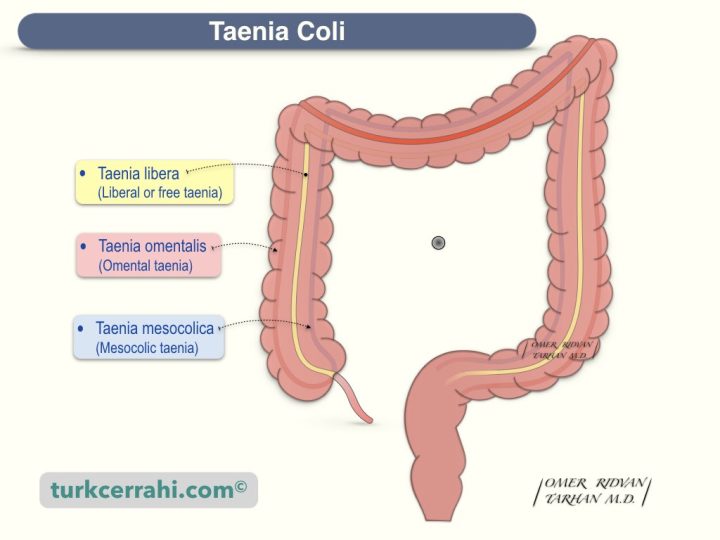
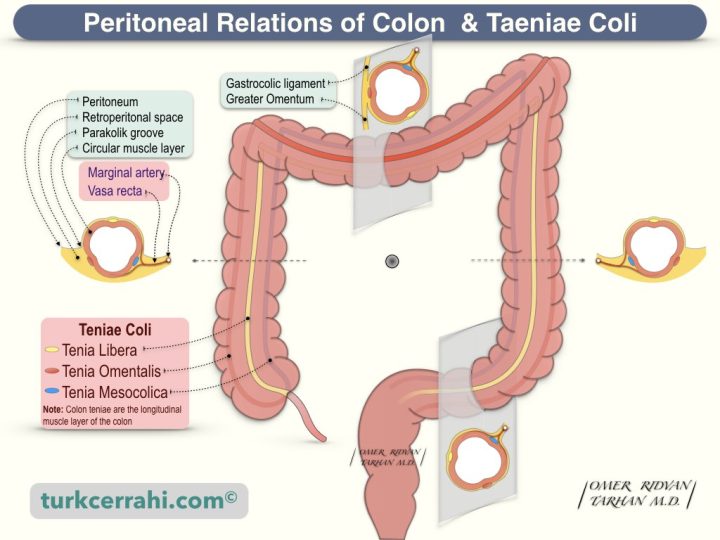
- Taeniae Coli (pl.) (Taenia Coli (sing.): The longitudinal (external) muscle layer of the colon is arranged in 3 separate bands (with 120 degrees intervals). The taeniae begin at the beginning of the colon (at the base of the cecum, at the root of the appendix), disperse in the rectum, and surround the rectum and anus. The names of these three taeniae are;
- Free taenia (taenia libera)
- Mesocolic taenia (tenia mesocolica)
- Epiploic taenia (taenia omentalis)
- Haustura Coli: Sacculation in the colon (except the rectum), which give the colon its segmented appearance.
- Mucosal Villi: Mucosal villi (small, finger-like projections) found in the small intestine are not found in the colon.
- Function: Small intestine principally absorbs digested nutrients whereas the large intestine absorbs water and electrolytes.
4. Peritoneal relations of colon and taeniae coli
5. Cecum
The cecum is the first and widest portion of the colon. It is in the right lower quadrant of the abdomen (right iliac fossa), with the appendix at its base. The cecum is relatively mobile. The ileum opens into the cecum on the medial wall of the cecum. As the largest section of the large intestine, the cecum is the most resistant to obstruction and the most susceptible to perforation. The three taeniae unite at the base of the cecum, and the appendix originates from here.
Ileocecal Valve (Ileocecal Valve)
The ileocecal valve is a unidirectional sphincter between the ileum and the cecum, preventing the reflux of large intestine contents (stool) into the ileum; it is also known as the Bauhin valve or Tulp valve. The ileocecal valve relaxes as the small intestine expands, allowing the ileum's contents to pass into the cecum (colon). When the colon is distended, the tone of the ileocecal valve increases further. Thus, the contents of the colon cannot return to the small intestine.
The ileocecal valve has an anti-diarrheal effect. In massive small bowel resection, preserving the ileocecal valve reduces short bowel syndrome and malabsorption.
The ileocecal valve is competent in 75 percent of individuals. If the ileocecal valve is competent, the risk of closed-loop obstruction and perforation increases. In this case, there is usually no air in the small intestine on X-rays.
Visualization of the ileocecal valve and appendix orifice indicates that the cecum has been reached on colonoscopy (i.e., all colon segments have been reached).
Caecus means blind in Latin. Other names of the ileocecal valve are the Bauhin valve, Tulp or Tulpius valve, Varolius valve, ileal valve, colic valve, and ileocolic valve.
6. Appendix (Appendix Vermiformis)
The appendix is a worm-shaped (vermiform) extension of the cecum (a thin, blind tube). Its length is about 5–10 cm (maybe 1–25 cm). A healthy appendix's diameter does not exceed 6 mm.
The origin of the appendix is relatively constant, where the three taeniae fuse at the base of the cecum (posterior to McBurney's point). However, other parts of the appendix are mobile, so it can be found in different positions: retrocecal (most), pelvic, subcecal, preileal, and postileal. The appendix can be reached during an appendectomy by following the tenia anterior to the cecum (taenia libera).
7. Ascending Colon
The ascending colon is the segment of the colon after the cecum, approximately 12.5–20 cm long, that ascends upward (to the liver), makes a sharp turn to the left under the right lobe of the liver (hepatic flexure), and goes to the spleen (transverse colon). The ascending colon, like the descending colon, is considered retroperitoneal because the peritoneum only covers the medial, lateral, and anterior parts of the ascending colon.
The hepatic flexure (right colic flexure) is located lateral to the gallbladder, anterior to the lower pole of the right kidney, and the second (descending) part of the duodenum.
8. Transverse Colon
The transverse colon has a downward convexity that starts from the hepatic flexure and extends to the splenic flexure. It is 40–50 cm long. The transverse colon is completely intraperitoneal, and the most mobile part of the colon has a mesentery (transverse mesocolon).
The transverse mesocolon divides the abdominal cavity into two compartments, the supramesocolic and inframesocolic spaces (compartments). Thus, the transverse mesocolon serves as a natural barrier against the spread of peritonitis and abscess.
The gastrocolic omentum (ligament) connects the anterosuperior portion of the transverse colon to the stomach's greater curvature. During colonoscopy, the gastrocolic ligament creates a triangular appearance inside the transverse colon.
When the gastrocolic ligament is opened, the bursa omentalis (lesser sac) is entered. In other words, the posterior surface of the stomach and the pancreas are exposed. For instance, the gastrocolic ligament is opened to inspect the stomach's posterior surface in cases of gastric injuries or to perform a distal pancreatectomy.
The Splenic Flexure (Left Colic Flexure): The transverse colon is attached to the lower part of the spleen (splenocolic ligament) and the diaphragm (phrenicocolic ligament) on the left side. It then makes a sharp downward turn. The splenic flexure is higher and deeper than the hepatic flexure. The splenic flexure is the most fixed part of the large intestine after the rectum.
9. Descending Colon
The descending colon starts from the splenic flexure and descends to the sigmoid colon at the level of the greater pelvis entrance. It is about 25–30 cm in length. It descends anteriorly to the kidney and slightly medially. As the peritoneum covers only the lateral, anterior, and medial surfaces of the descending colon, it is retroperitoneal (like the ascending colon). The descending colon is deeper and thinner than the ascending colon.
10. Sigmoid Colon
The sigmoid colon is the narrowest and most mobile segment of the large intestine, which is between the descending colon and the rectum. Because of its narrow diameter, the sigmoid colon is the most vulnerable segment of the large intestine to obstruction.
The sigmoid colon begins at the entrance to the greater pelvis and terminates at the level of the 3rd sacral vertebra (rectosigmoid junction; sacral promontory for some sources).
The sigmoid colon consists of two parts, the iliac (fixed) and pelvic (mobile, mesenteric). The sigmoid colon is about 40 cm long. The middle part of the sigmoid colon may extend into the right lower quadrant.
Etymology: Sigma is the eighteenth letter of the Greek alphabet (uppercase: Σ, lowercase: σ, en of word: ς). The sigmoid colon is similar to the lowercase sigma at the end of the word (ς).
Sigmoid Colon Mesentery
The mobile (pelvic) part of the sigmoid colon has an omega-shaped (Ω) mesentery (long but narrow-based). Therefore, the most common site of volvulus is the sigmoid colon (2nd cecum).
The sigmoid mesocolon adhesion line to the posterior abdominal wall is in an inverted “V” shape. The apex is around the bifurcation of the left common iliac artery. The left leg is medial to the left psoas muscle. The right leg descends into the pelvis and ends in front of the third sacral segment in the midline.
Intersigmoid Fossa (Recess): When the sigmoid colon is tilted medially, the depression in the middle of the line where the meson attaches to the posterior abdominal wall is called the intersigmoid fossa. It is more pronounced in fetal life. The left ureter descends behind this fossa. The intersigmoid fossa can be used as a landmark to locate the left ureter and avoid injury.
Rectosigmoid Junction
The rectosigmoid junction can be identified by six characteristics (more precisely, where the sigmoid colon ends and the rectum begins).
- The disappearance of colon haustra (rectum is straight)
- Narrowing of the intestinal lumen
- The disappearance of the sigmoid mesocolon
- Dispersion of taeniae and covering the rectum in a single sheath.
- The disappearance of epiploic appendices
- Mucosal difference: The rectal mucosa is smooth and flat, and there are 3 valves (Houston valves). There are prominent mucosal folds in the sigmoid colon mucosa.
11. Rectum
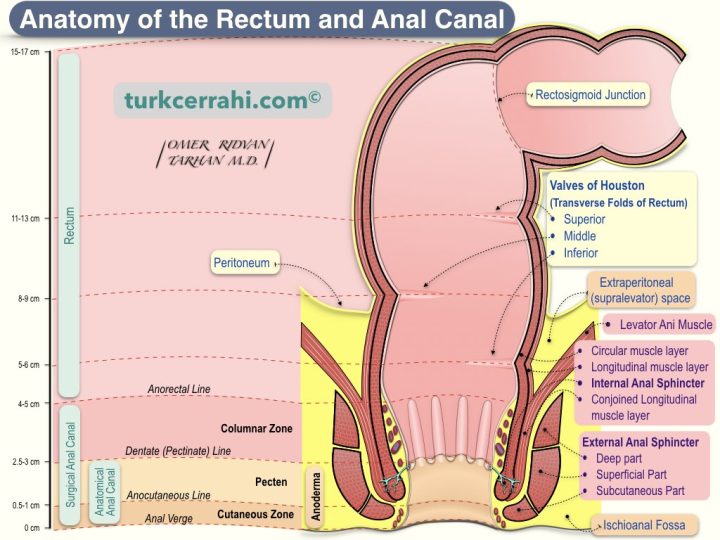
The rectum begins after the sigmoid colon (at the level of SIII, according to some sources, the sacral promontory) and terminates at the anus. The anorectal junction refers to the point where the anal canal meets the rectum. This junction is anatomically defined externally by the puborectal and pelvic floor muscles and internally by the dentate line.
The word "rectum" comes from Latin (rectus), meaning straight. There are three mucosal folds in the rectum (upper left, middle right, and lower left), called the valves of Houston. The rectum is 12 cm long. The middle part of the rectum is wider (ampulla recti).
The Function of the Rectum: Stool coming from the sigmoid colon is stored in the rectum before defecation. When the rectum is distended, the internal and external anal sphincters relax (rectoanal inhibitory reflex), the rectum contracts and shortens, and defecation occurs. If a person voluntarily holds back his or her stool (external sphincter), the stool returns to the sigmoid colon, and the water in the stool continues to be absorbed, causing the stool to harden even more.
12. Anal Canal
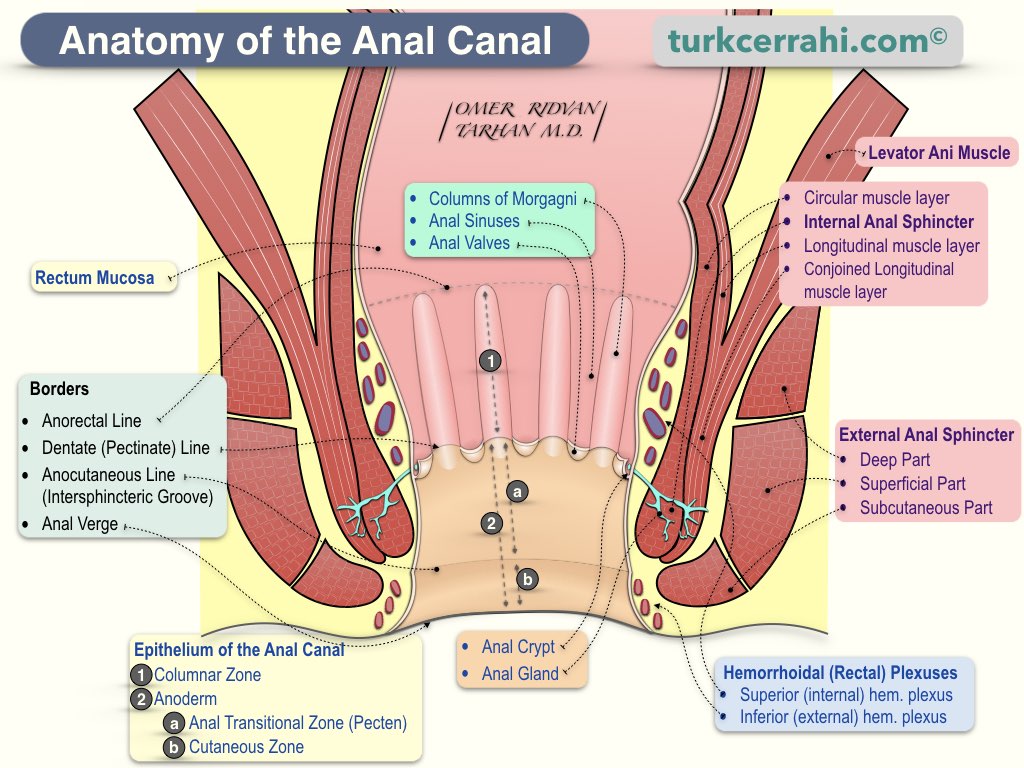
The anal canal is the last part of the large intestine, with a length of 4-5 cm. It is between the rectum and the anal verge (anal orifice, anus).
The keratinized, pigmented perianal skin around the anal verge has skin appendages (hair, sweat, and sebaceous glands). The anal canal skin (anoderm) above the anal verge is also pigmented and keratinized and is pain-sensitive like the skin, but without skin appendages.
Surgical Anal Canal
The upper border between the anal canal and the rectum is accepted as the anorectal ring (anorectal angle). Its average length is 4-5 cm. ⅔ of the anal canal is above the dentate line, and ⅓ is below the dentate line.
Anatomical Anal Canal
The upper border of the anal canal is considered the dentate line (pectinate line). Its average length is 2.5-3 cm.
13. Ligaments of the Colon
Gastrocolic Ligament: The part of the greater omentum between the greater curvature of the stomach and the transverse colon is called the gastrocolic ligament. By opening the gastrocolic ligament, it is accessed the posterior wall of the stomach, and the anterior surface of the pancreas, namely the lesser sac.
Splenocolic Ligament: The firm peritoneal connection between the lower pole of the spleen and the splenic flexure.
Phrenicocolic Ligament: The connection between the splenic flexure and the diaphragm
14. Arteries of the Colon
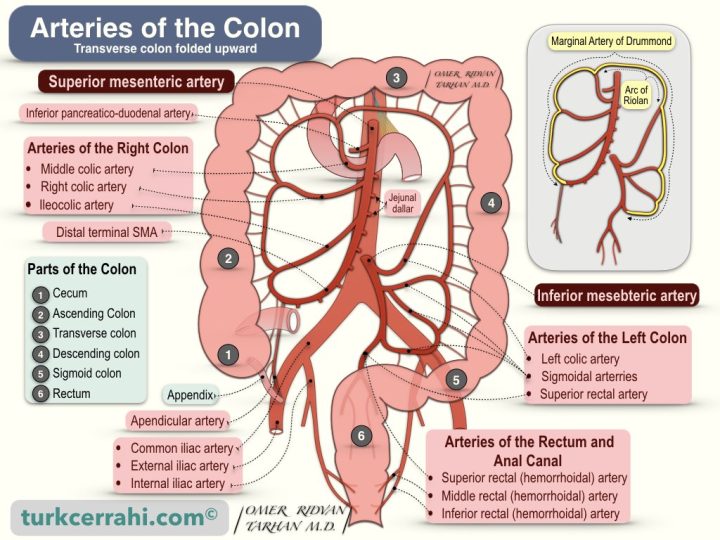
The arteries of the colon include the last three branches of the superior mesenteric artery and all branches of the inferior mesenteric artery.
- Branches of Superior Mesenteric Artery: All branches of superior mesenteric artery are listed below for easier understanding, the last three branches are related to the colon.
- Inferior Pancreaticoduodenal Artery
- Jejunal and Ileal branches
- Middle Colic Artery supplies the transverse colon
- Right Colic Artery supplies the ascending colon
- Ileocolic Artery supplies the terminal ileum, appendix, cecum, and proximal ascending colon.
- Branches of the Inferior Mesenteric Artery: All branches supply the left colon. Respectively;
- Left Colic Artery supplies the descending colon
- Sigmoidal Branches supply the sigmoid colon
- Superior Rectal Artery supplies the proximal rectum
Ileocolic Artery
It is the last branch of the superior mesenteric artery. The ileocolic artery also divides into two branches.
- The superior branch ascends, anastomose with the descending branch of the right colic artery.
- The inferior branch gives cecal branches, appendicular artery, and ileal branches.
Right Colic Artery
The right colic artery supplies the ascending colon. As it approaches the colon, it divides into two branches.
- The descending branch anastomoses with the ascending branch of the ileocolic artery.
- The ascending branch anastomoses with the right branch of the middle colic artery.
Middle Colic Artery
The middle colic artery runs inside the transverse mesocolon and divides into two branches as it approaches the colon.
- The right branch of the middle colic artery anastomoses with the ascending branch of the right colic artery
- The left branch of the middle colic artery anastomoses with the ascending branch of the left colic artery (Arc of Riolan).
The Arc of Riolan, also called the Riolan anastomosis, is part of the marginal artery of Drummond. The arc of Riolan, also known as the meandering mesenteric artery or the central mesenteric artery, is an important arterial connection between the superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA). This connection is significant because it allows for collateral blood flow between the two arteries, which supply blood to the small and large intestines.
In cases of arterial occlusion or stenosis in one of these arteries, the arc of Riolan can provide an alternative route for blood flow to the affected area of the intestine, preventing ischemia (insufficient blood supply) and potential tissue damage.
Left Colic Artery
The left colic artery is the first branch of the inferior mesenteric artery. The left colic artery divides into two branches in the retroperitoneum.
- The ascending branch supplies the proximal descending colon and the distal transverse colon. The ascending branch anastomoses with the left branch of the middle colic artery to form the Riolan arch.
- The descending branch supplies the distal descending colon, and anastomosis with the first sigmoid artery branch.
Sigmoidal Arteries
The sigmoid artery typically consists of 2–4 branches that run in the sigmoid mesocolon. The uppermost (superior) sigmoid artery anastomoses with the descending branch of the left colic artery. The sigmoidal arteries supply the distal descending colon and the sigmoid colon.
Rectal Arteries
Superior Rectal (Hemorrhoidal) Artery
The superior rectal artery is the terminal branch of the inferior mesenteric artery. The superior rectal artery enters the pelvis on its medial side and passes through the sigmoid colon mesentery. It divides into two branches at the level of the S3 vertebra, giving small branches to the right and left of the rectum, and descends to the level of the internal anal sphincter. The superior rectal artery supplies the proximal part of the rectum.
Middle Rectal (Hemorrhoidal) Artery
The middle rectal artery is a branch of the internal iliac artery that supplies the distal rectum.
Inferior Rectal (Hemorrhoidal) Artery
The inferior rectal artery is a branch of the internal pudendal artery, which, in turn, is a branch of the internal iliac artery. The inferior rectal artery supplies the anal canal, anal muscles, anal area, and surrounding gluteal skin. The internal pudendal artery supplies blood to the perineum, which is the region between the anus and the external genitalia. Specifically, it provides blood supply to the external genitalia, including the clitoris, labia majora, and scrotum, as well as the anal canal, perianal skin, and the muscles and structures in the pelvic floor.
There is a well-developed network between the terminal branches of the superior, middle, and inferior rectal arteries. This network makes the rectum resistant to ischemia.
Marginal Artery of Drummond
The arteries of the colon anastomose with each other at the colon's margin before entering the colon, forming Drummond's marginal artery. At the edge of the splenic flexure, the marginal artery of Drummond is called the arc of Riolan. Therefore, the arc of Riolan is an important arterial connection between the superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA).
15. Veins of the Colon
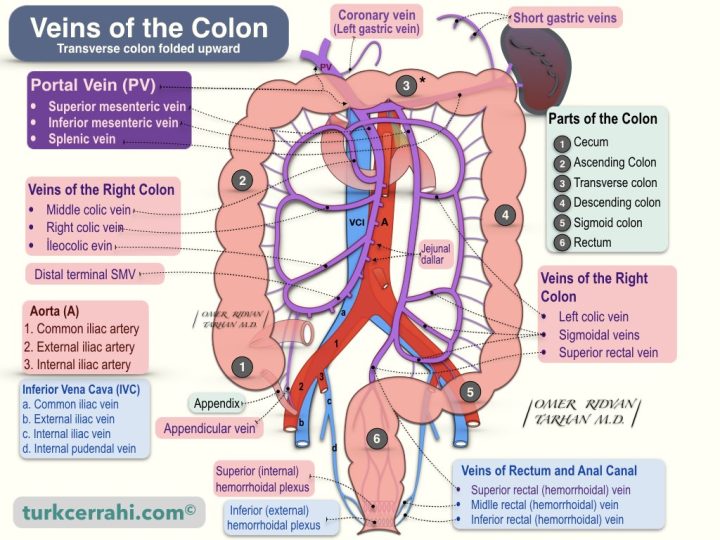
Except for the lower part of the rectum, the venous drainage of the stomach, small and large intestines, spleen, pancreas, and gallbladder is to the liver via the portal vein.
The blood from the portal vein flows into the liver through specialized blood vessels called hepatic sinusoids. The hepatic sinusoids are a network of capillaries that are lined by specialized cells called hepatic stellate cells and Kupffer cells. These cells help filter and process the blood that flows through the sinusoids. After passing through the hepatic sinusoids, the blood from the portal vein is collected by the hepatic veins, which drain into the inferior vena cava.
The venous drainage of the colon occurs via both the superior and inferior mesenteric veins.
The superior mesenteric vein drains blood from the small intestine, ascending colon, and transverse colon, while the inferior mesenteric vein drains blood from the descending colon, sigmoid colon, and rectum.
Superior Mesenteric Vein
The superior mesenteric vein is like a venous replica of the superior mesenteric artery. The superior mesenteric vein drains the jejunal, ileal, ileocolic, right, and middle colic veins. In other words, the blood from the jejunum, ileum, cecum, ascending colon, and transverse colon drains into the superior mesenteric vein.
The superior mesenteric vein arises from the right iliac fossa and ascends, passing in front of the horizontal part of the duodenum and then behind the pancreatic neck. At the level of the upper edge of the pancreas, the splenic vein joins the superior mesenteric vein, and together they form the portal vein (at the level of the L2 vertebra). The inferior mesenteric vein drains into the splenic vein. Sometimes the superior mesenteric vein, inferior mesenteric vein, and splenic vein unite at the same junction (trifurcation).
Inferior Mesenteric Vein
The inferior mesenteric vein drains blood from the rectum, sigmoid colon, and descending colon.
The inferior mesenteric vein is like a venous replica of the inferior mesenteric artery. The inferior mesenteric vein begins in the rectum as the superior rectal vein; as it ascends, it receives the sigmoidal veins and the left colic vein. The inferior mesenteric vein drains into the splenic vein. The splenic vein joins with the superior mesenteric vein to form the portal vein.
Superior Rectal (Hemorrhoidal) Vein
The superior rectal vein drains the rectum (via the superior (internal) hemorrhoidal plexus). The inferior mesenteric vein is formed by the convergence of several veins, including the left colic vein, the sigmoid veins, and the superior rectal vein.
Middle Rectal (Hemorrhoidal) Vein
The middle rectal vein, along with the inferior rectal vein, drains blood from the anal canal, anal muscles, anal region, and surrounding gluteal skin (via the inferior (external) hemorrhoidal plexus). It joins the internal iliac vein.
Inferior Rectal (Hemorrhoidal) Vein
The inferior rectal vein, along with the middle rectal vein, drains blood from the anal canal, anal muscles, anal region, and surrounding gluteal skin (via the inferior (external) hemorrhoidal plexus). The inferior rectal vein, which begins as several branches, joins to form the internal pudendal vein. After receiving the middle rectal vein and other small veins, the internal pudendal vein becomes the internal iliac vein.
Rectal Venous Plexus (Hemorrhoidal Plexus)
The veins draining the distal rectum and the anus arise from two venous plexuses.
- Internal (superior) hemorrhoidal (rectal) plexus
- External (inferior) hemorrhoidal (rectal) plexus
The communications between the superior and inferior hemorrhoidal plexuses are dilated in portal hypertension, acting as portosystemic collaterals.
The internal hemorrhoidal plexus is located submucosal and just above the anorectal line. It drains into the superior hemorrhoidal (rectal) vein > inferior mesenteric vein > portal system.
Dilatation and elongation of the internal hemorrhoidal veins cause internal hemorrhoidal disease. Because the caval vessels lack venous valves, portal hypertension is exactly reflected in the internal hemorrhoid plexus. Therefore, there is a tendency to develop internal hemorrhoidal disease.
The external hemorrhoidal plexus, located outside the muscular layer and below the anorectal line, drains into two veins:
Inferior hemorrhoidal (rectal) vein > internal pudendal vein > internal iliac vein > caval system
Middle hemorrhoidal (rectal) vein > internal iliac vein > caval system
Enlargement of the external hemorrhoidal plexus causes external hemorrhoidal disease.
16. Lymph Vessels and Nodes of The Colon
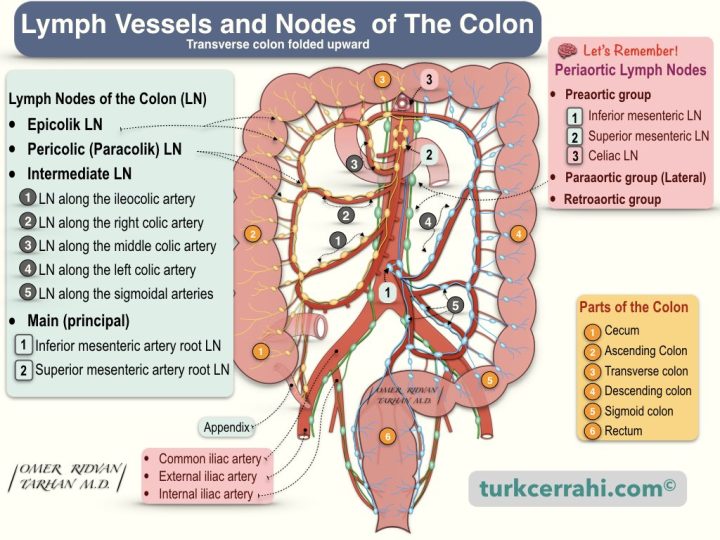
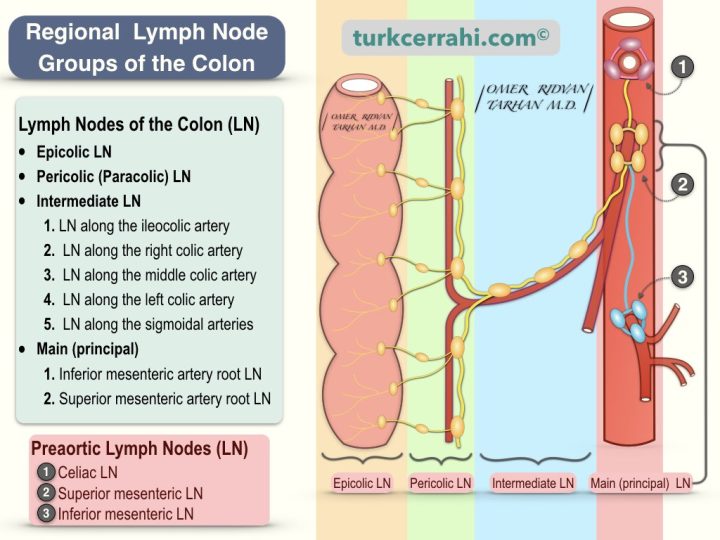
The lymphatic flow of the gastrointestinal tract in the abdomen begins in the tissue and ends in large bundles of lymph nodes at the root of the anterior branches of the abdominal aorta (preaortic lymph nodes).
Preaortic lymph nodes are divided into three groups:
- Celiac lymph nodes
- Superior mesenteric lymph nodes and
- Inferior mesenteric lymph nodes
Inferior mesenteric lymph nodes > drain into superior mesenteric lymph nodes > these drain into celiac lymph nodes, which in turn drain into cisterna chyli > which drain into left subclavian vein
The lymphatic drainage of the colon and the lymph node groups are arranged as follows, respectively:
- Submucosal and Subserosal Lymphatic Plexus (interconnected)
- Epicolic Lymph Nodes (Located in the colon wall, below the serosa, and in the epiploic appendices. Most numerous in the sigmoid colon)
- Paracolic Lymph Nodes (Lymph nodes around their corresponding arterial arcades)
- Intermediate Lymph Nodes (Through segmental colonic vessels, i.e., lymph nodes around ileocolic, right colic, middle colic, left colic, and sigmoidal arteries)
- Main (Principal) Lymph Nodes
- Lymph nodes around the Superior Mesenteric Artery Root
- Lymph Nodes around the Inferior Mesenteric Artery Root
17. Nerves of the Colon
The large intestine is controlled by two nervous systems (intrinsic, and extrinsic)
- Enteric Nervous System (Intrinsic)
- Autonomic Nervous System (Extrinsic)
- Sympathetic Nervous System (Thoracolumbar Division)
- T11-12 > Sympathetic chain ganglion > Superior mesenteric artery ganglion > Right colon
- L1-2 > sympathetic chain ganglion > inferior mesenteric artery ganglion > Left colon
- Lumbar splanchnic nerves, superior and inferior hypogastric plexuses > Rectum
- Parasympathetic Nervous System (Craniosacral Division)
- Vagus nerve (X. Cranial Nerve) > Right Colon (cecum, ascending colon, transverse colon)
- Sacral 2-4 nerves > pelvic splanchnic nerves (n. erigentes) > Left Colon (descending colon, sigmoid, rectum)
- Sympathetic Nervous System (Thoracolumbar Division)
The sympathetic innervation (nerves) of the colon inhibits (reduces) colonic peristalsis and secretions and causes contraction of the ileocolic and rectal sphincters.
The parasympathetic innervation (nerves) of the colon stimulates (increases) colonic peristalsis and secretions while relaxing the ileocolic and rectal sphincters.
Visceral sensory fibers (visceral afferent fibers), including those in the colon, are carried by both sympathetic and parasympathetic nerves.
- Visceral sensory fibers accompanying the sympathetic fibers (carried within the sympathetic nerves) transmit pain.
- Visceral sensory fibers accompanying the parasympathetic fibers (carried within the parasympathetic nerves) carry the impulses formed in the chemoreceptors and baroreceptors, they carry information about reflex activity and physiological processes.