Diaphragm
1. Definition
The diaphragm (thoracic diaphragm) is a large, dome-shaped muscle that separates the thoracic and abdominal cavities and is the primary muscle involved in respiration.
By increasing intra-abdominal pressure, the diaphragm aids in coughing, sneezing, vomiting, crying, defecation, urination, and childbirth.
Terminal lymphatic capillaries, called lacunae, located in the diaphragm, absorb fluid from the peritoneal cavity. Peritoneal fluid enters the lacunae through small openings called stomata on the free surface of the mesothelium. In other words, lymphatic stomata are small openings of lymphatic capillaries on the free surface of the mesothelium.
2. Openings
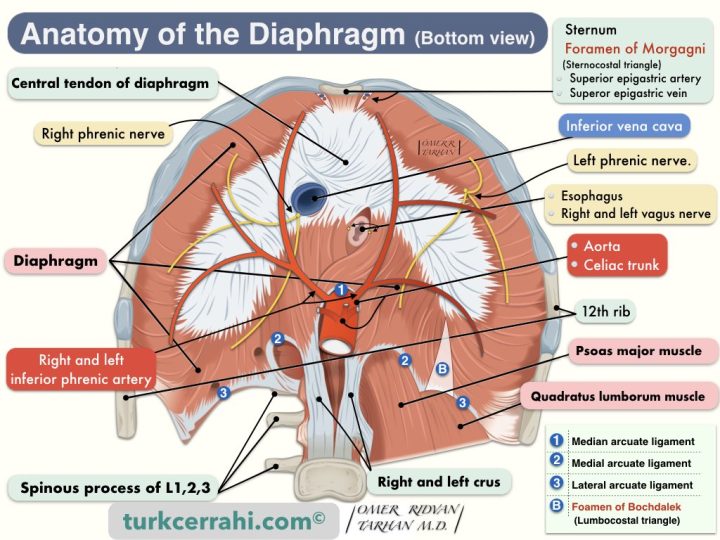
The diaphragm separates the abdomen from the chest. Many structures pass between the abdominal and thoracic cavities through the diaphragm or its edges. In other words, the diaphragm has several openings called hiatuses.
Diaphragmatic Openings (Hiatus) and Structures Pass-Through
- Esophageal Hiatus
- Esophagus
- Anterior and posterior vagal trunk
- Hiatus of Inferior Vena Cava
- Inferior Vena Cava
- Right Phrenic Nerve
- Aortic Hiatus
- The aorta
- Thoracic Duct (Ductus Thoracicus)
- Azygos Vein
- Hemiazygos Vein
- Foramen of Morgagni (Sternocostal Triangle, Larrey’s Space)
- Right and Left Superior Epigastric Artery and Vein
- Foramen of Bochdalek (Lumbocostal Triangle, normally absent or closed)
- Other Structures Passing Through the Diaphragm
- Greater and lesser splanchnic nerves (pass through the left crus)
- Hemyazygos vein usually passes through the aortic hiatus, sometimes through the left crus.
- Right and Left Sympathetic Truncus: On both sides, they pass behind the median arcuate ligament.
- Left Phrenic Nerve: The right phrenic nerve crosses the diaphragm (usually) to the right of the inferior vena cava. The left phrenic nerve passes over the pericardium of the left ventricle, perforates the diaphragm, and is distributed on the lower surface of the diaphragm.
3. Is the diaphragm muscle voluntary or involuntary?
The diaphragm is a musculomembranous (musculotendinous) structure. The middle is membranous (central tendon), and the edges are striated muscle (i.e., skeletal muscle). However, the diaphragm muscle and breathing normally work involuntarily (automatically). Sometimes, voluntary breathing also comes into play. For example, talking, singing, laughing, deep breathing, and whistling
4. Diaphragmatic Hernias
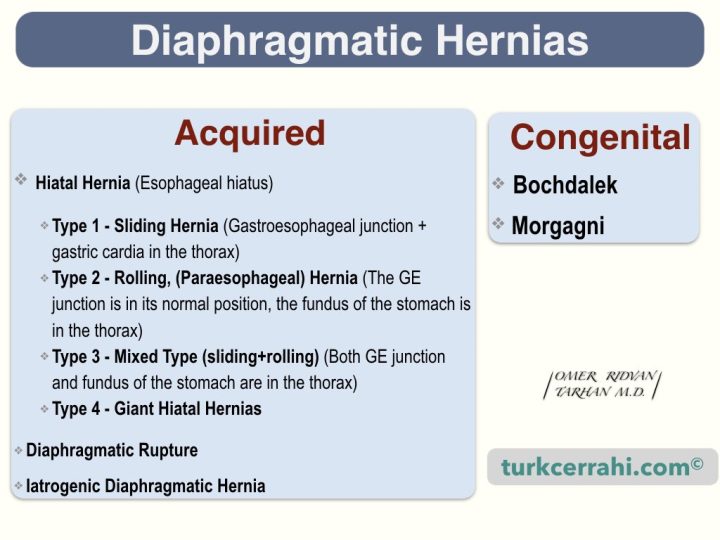
Acquired Diaphragmatic Hernias
- Hiatal Hernia (through the esophageal hiatus)
- Type 1, sliding hernia (gastroesophageal junction + gastric cardia in the thorax)
- Type 2, rolling (paraesophageal) hernia (The GE junction is in its normal position, the fundus of the stomach is in the thorax)
- Type 3, mixed type, sliding+rolling (Both GE junction and fundus of the stomach are in the thorax)
- Type 4, giant hiatal hernias: The GE junction is in its normal position, most of the stomach, colon, omentum, and spleen in the thorax
- Diaphragmatic Rupture: Usually occurs with penetrating injury. The hernia may enlarge and give symptoms months and years later.
- Iatrogenic Diaphragmatic Hernia: Due to previous abdominal and thoracic surgeries; such as esophagectomy, gastrectomy, nephrectomy, lung lobectomy, and liver resections.
Congenital Diaphragmatic Hernias
There are two types of congenital diaphragmatic hernias.
- Morgagni hernia occurs just to the right and behind the sternum (remember, the inferior epigastric artery and vein pass through the sternocostal triangle).
- Bochdalek Hernias are posterior to the diaphragm and usually to the left (85%), because the left pleuroperitoneal canal (diaphragm) closes later.
5. Diaphragm Paralysis
Diaphragmatic paralysis is uncommon and can be unilateral or bilateral. Diaphragm paralysis can cause dyspnea and impair ventilation (breathing). The clinical symptoms are more prominent in bilateral diaphragm paralysis, while unilateral diaphragm paralysis is mostly asymptomatic
The etiology is unknown (idiopathic) in many cases. Unilateral paralysis is not uncommon following phrenic nerve injury during cardiac surgery, cervical spondylosis, pneumonia, herpes zoster neuritis, or mediastinal compressive tumors. Bilateral paralysis is usually part of motor neuron disease (Guillain–Barré syndrome), myopathies (polymyositis, dermatopolymyositis), and muscular dystrophy.
Diaphragm paralysis is usually suspected based on a chest x-ray and clinical examination.
Treatment is often unnecessary in unilateral cases, but in more severe cases, nocturnal positive pressure ventilation, diaphragmatic pacing, and diaphragmatic plication should be considered.