Anatomy of the Extrahepatic Bile Ducts
1. Extrahepatic Bile Ducts
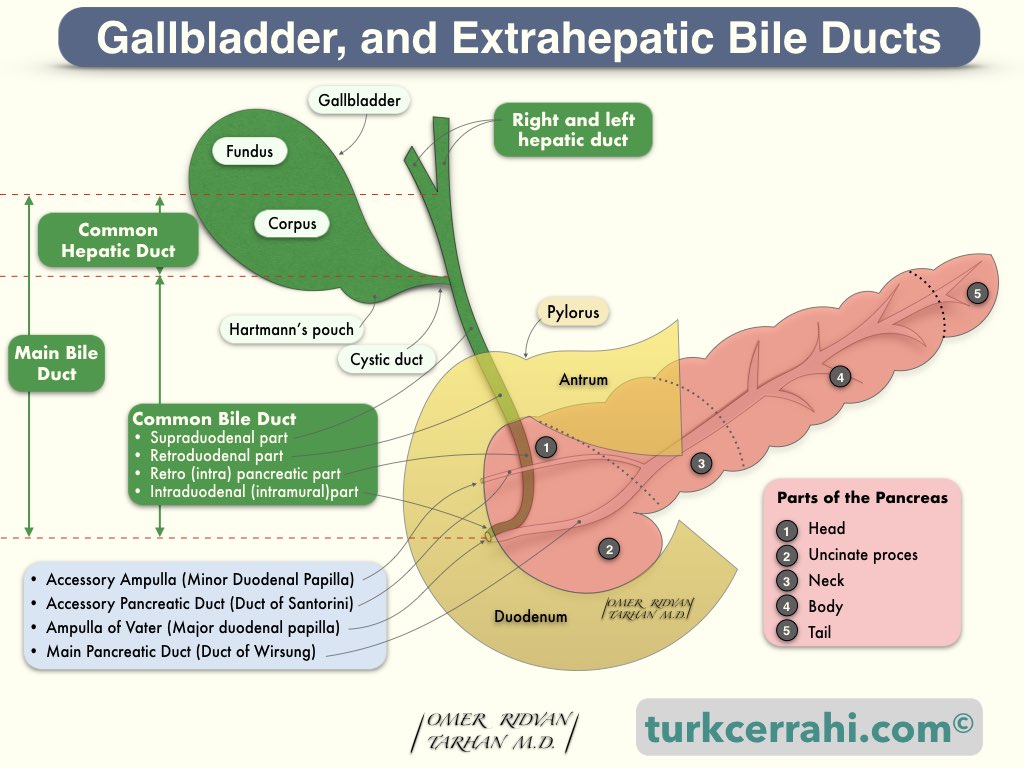
Extrahepatic bile ducts consist of the right and left hepatic ducts, the common hepatic duct, the cystic duct, and the common bile duct. The left hepatic duct is longer than the right (~1.7 cm vs ~0.9 cm). The common hepatic duct is 1-4 cm long.
The common hepatic duct joins the cystic duct to form the common bile duct (CBD).
2. Cystic Duct
The cystic duct is approximately 3 mm in diameter. Its length varies between 2-4 cm, depending on the type of union with the common hepatic duct. The cystic duct usually (80%) joins the main hepatic duct above the duodenum. Rarely, the cystic duct may be absent.
The point of insertion of the cystic duct into the CHD is variable. According to a study of MR cholangiography, the level of the union of the cystic duct to the bile duct was proximal in 29%, middle in 49%, and distal in 20%. In the same study, the cystic duct orifice was 50% on the lateral surface of the bile duct, 19% posterior, 15% anterior, and 14% medial. In other words, the cystic duct usually enters the CHD from the right lateral side, roughly halfway between the hepatic confluence and the ampulla of Vater. Rarely, the cystic duct opens directly into the duodenum.
Main Variations in Cystic Duct
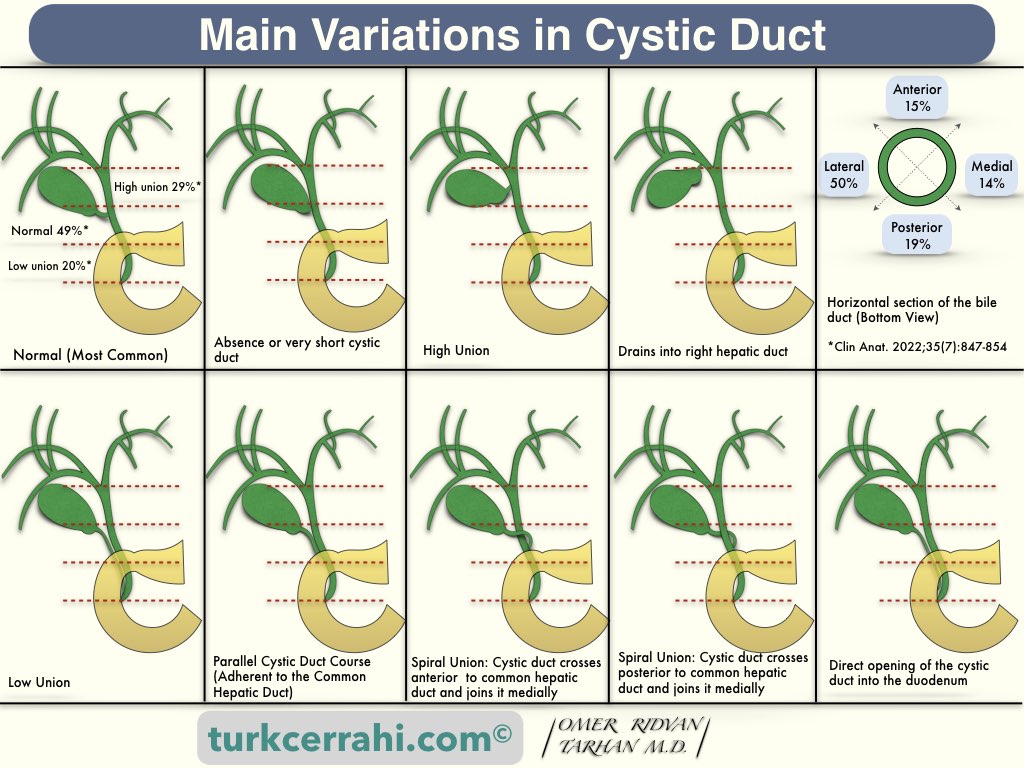
- Absence or very short cystic duct
- High union with common hepatic duct
- Drains into the right hepatic duct
- Low union with common hepatic duct
- Parallel cystic duct course (adherent to common hepatic duct)
- Spiral union with common hepatic duct (anterior, posterior, or medial)
- Direct opening of the cystic duct into the duodenum (very rare)
3. Common Bile Duct (CBD)
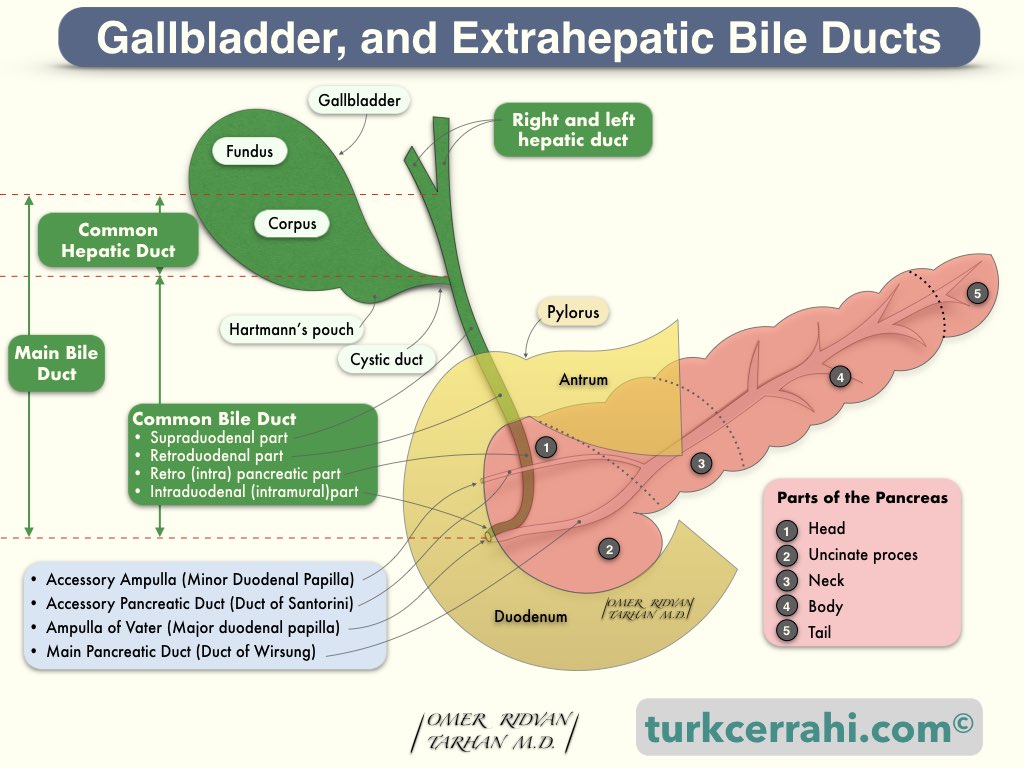
The length of the common bile duct varies between 5-15 cm (average: 7 to 11 cm) depending on the union point of the cystic duct.
The external diameter of the common bile duct is 5-10 mm. The internal diameter of the common bile duct measured by ultrasound is considered normal up to 6-7 mm. In patients without a history of cholecystectomy, an inner diameter of the bile duct greater than 7 to 8 millimeters indicates obstruction. Following cholecystectomy, asymptomatic bile duct dilatation of up to 10 mm is considered normal.
The main bile duct can be divided into 4 parts,
- Supraduodenal (above the duodenum)
- Retroduodenal (behind the duodenum)
- Pancreatic (sometimes behind the pancreas, sometimes inside)
- Intramural (inside the wall of the duodenum)
As the common hepatic duct descends further, it joins the cystic duct to form the common bile duct (CBD). The common bile duct joins with the pancreatic duct to form the Ampulla of Vater. The ampulla of Vater opens the descending part of the duodenum at the major duodenal papilla (also called the papilla of Vater). The ampulla of Vater protrudes into the duodenum, forming the major duodenal papilla. The distance between the papilla and the pylorus is approximately 10 cm.
Pancreaticobiliary Junction Types
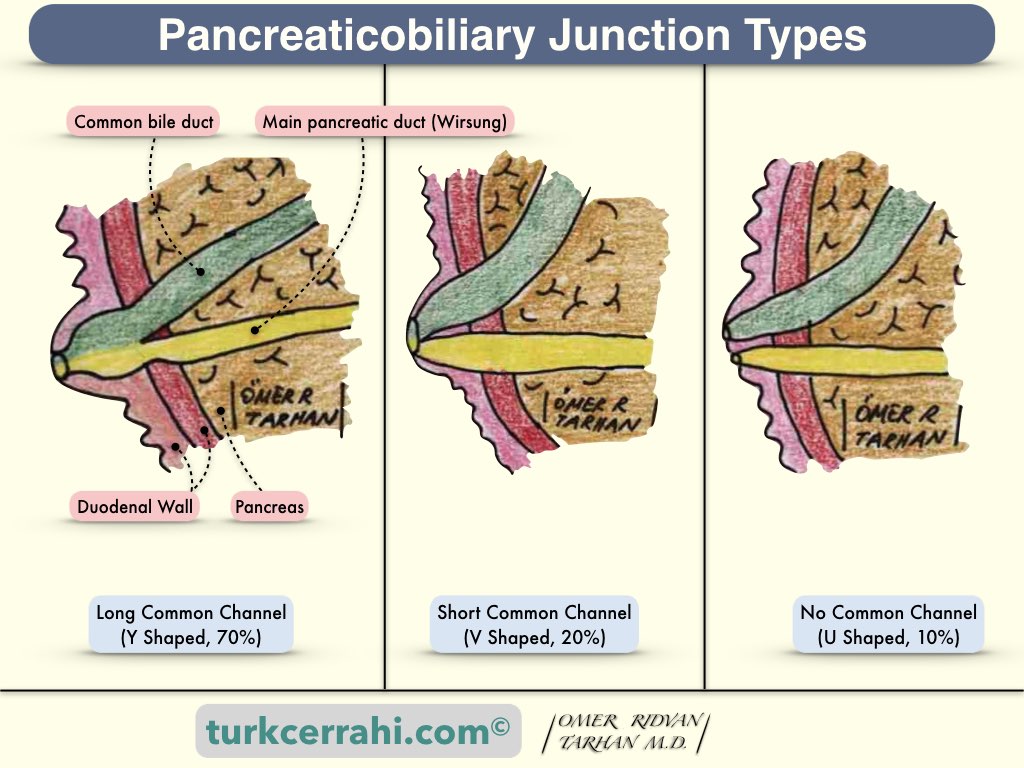
The smooth muscle structure that surrounds the ampulla of Vater, the end of the common bile duct, and the Wirsung canals is called the sphincter of Oddi. This sphincter is contracted during fasting and allows bile to fill the gallbladder. When we eat, the sphincter of Oddi relaxes and allows bile from the gallbladder to pass into the duodenum.
4. Sphincter of Oddi
The sphincter of Oddi is the smooth muscle sphincter of the ampulla of Vater and regulates the flow of bile and pancreatic juice. The sphincter of Oddi is about 4 to 6 mm in length. The sphincter's basal resting pressure is about 13 mmHg. The sphincter also shows phasic contractions with a frequency of four per minute and a duration of 8 seconds. Pressure may increase dramatically with phasic contractions, with an average amplitude of 130 mmHg.
When partially digested food reaches the duodenum, a peptide hormone called cholecystokinin (CCK) is secreted into the blood.
CCK relaxes the sphincter of Oddi and causes the gallbladder to contract and empty. Parasympathetic stimulation also causes relaxation of the sphincter of Oddi.
Sympathetic splanchnic stimulation increases sphincter pressure.
5. Arterial Blood Supply of Extrahepatic Bile Ducts
The extrahepatic bile duct receives arterial blood from the left and right hepatic arteries, the cystic artery, the proper hepatic artery, and the posterior superior pancreaticoduodenal artery. These arteries form the complex peribiliary vascular plexus. The two most important arteries to the supraduodenal bile duct run parallel to the duct at the 3-o’clock and 9-o’clock positions.
6. Venous Drainage of Extrahepatic Bile Ducts
Veins drain the hepatic ducts and the gallbladder and empty into hepatic vein branches within the liver. Venous drainage from the bile duct's lower portion drains directly into the portal vein.
Several small veins in the gallbladder bed empty directly into branches of hepatic veins in the liver parenchyma. In other words, the cystic vein is usually absent. When present, the cystic vein drains into the right branch of the portal vein, accompanying the cystic duct.
7. Lymphatic Drainage of Extrahepatic Bile Ducts
Lymphatic vessels from the hepatic ducts and upper common bile duct drain into the hepatic lymph nodes (around the hepatic artery) to drain into the celiac lymph nodes. Lymph from the lower bile duct drains into the lower hepatic nodes as well as the upper pancreatic lymph nodes.
Gallbladder and cystic duct lymphatic vessels drain primarily into the cystic duct node. The cystic duct node is located at the junction of the cystic duct and the common hepatic duct and drains into the hepatic lymph nodes and, eventually, the coeliac lymph nodes.
The cystic duct node is the sentinel lymph node of the gallbladder and is also called Lund’s node (the cystic lymph node of Lund) or Mascagni’s lymph node.
8. Innervation of Extrahepatic Bile Ducts
The nerve supply to the common bile duct and sphincter of Oddi is the same as for the gallbladder. The gallbladder and extrahepatic bile ducts receive parasympathetic, sympathetic, and sensory innervation.
- Parasympathetic nerve supply from the right vagus through its hepatic branch
- Sympathetic supply comes from T 7-9 through the celiac plexus.
- Sensory information from the gallbladder (pain of the biliary colic) passes through the splanchnic nerves via sympathetic afferent fibers. According to some other sources, sensory information is carried by the right phrenic nerve.
9. Histology of Extrahepatic Bile Ducts
Extrahepatic bile ducts are lined with columnar mucosa surrounded by a layer of connective tissue. Muscle fibers in the bile duct are sparse and discontinuous.