Pancreas Anatomy and Embryology
The pancreas is a retroperitoneal gland that secretes both hormones and digestive enzymes (endocrine - exocrine). It is 75-100 g in weight and 15-20 cm long.
- Pancreas Anatomy
- Parts of the Pancreas
- Pancreatic Duct Anatomy (And Embryology)
- Anatomic Variations of Pancreatic Ducts and Pancreas Divisum (Wirsung & Santorini)
- Anatomic Variations of Ampulla of Vater; Relations of Duct of Wirsung and Common Bile Duct
- Ampulla of Vater, Sphincter of Oddi, Papilla of Vater, Papilla Duodeni Minor
- Arterial Supply of the Pancreas
- Venous Drainage of the Pancreas
- Lymphatic Drainage of the Pancreas
- Innervation of the Pancreas
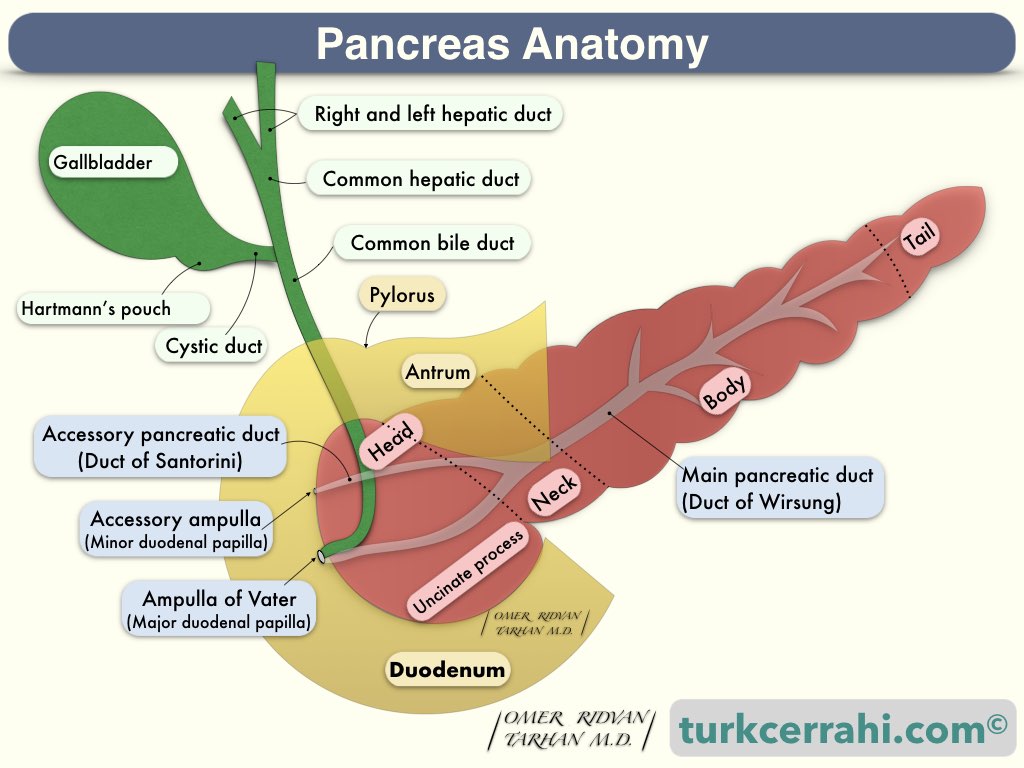
1. Pancreas Anatomy
- The pancreas is a retroperitoneal organ (75-100 g, 15-20 cm).
- The pancreas is a gland that secretes both hormones and digestive enzymes (endocrine and exocrine).
- The primary hormone secreted by the pancreas is insulin, which reduces blood sugar (glucose).
- Since the pancreas is a retroperitoneal organ, pancreatic pain radiates to the waist.
- The pancreas is behind the stomach
- It lies between the duodenum and the spleen (right and left).
Parts of the Pancreas
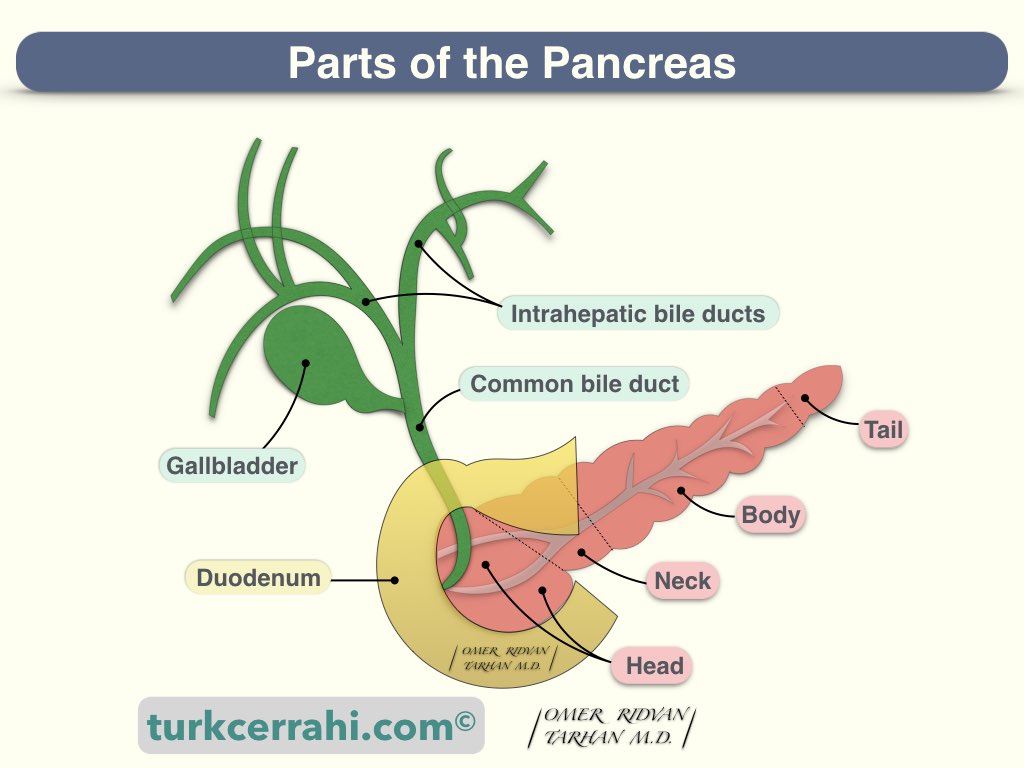
The head of the pancreas is the part attached to the duodenum. The head is at the L2 level and close to the midline, in front of the inferior vena cava.
The uncinate process is like a protuberance running down from the head. The uncinate process develops from the ventral pancreatic bud.
The neck of the pancreas is anterior to the superior mesenteric artery and vein.
The body of the pancreas: The splenic artery and vein pass through its posterior upper part. Because of this neighborhood, pancreatitis sometimes causes splenic vein thrombosis. Most of the pseudocysts develop in the body of the pancreas. The stomach and the transverse colon mesentery form the anterior wall of the pseudocyst.
The tail of the pancreas is close to the hilum of the spleen and can be injured during a splenectomy.
Pancreatic Duct Anatomy (And Embryology)
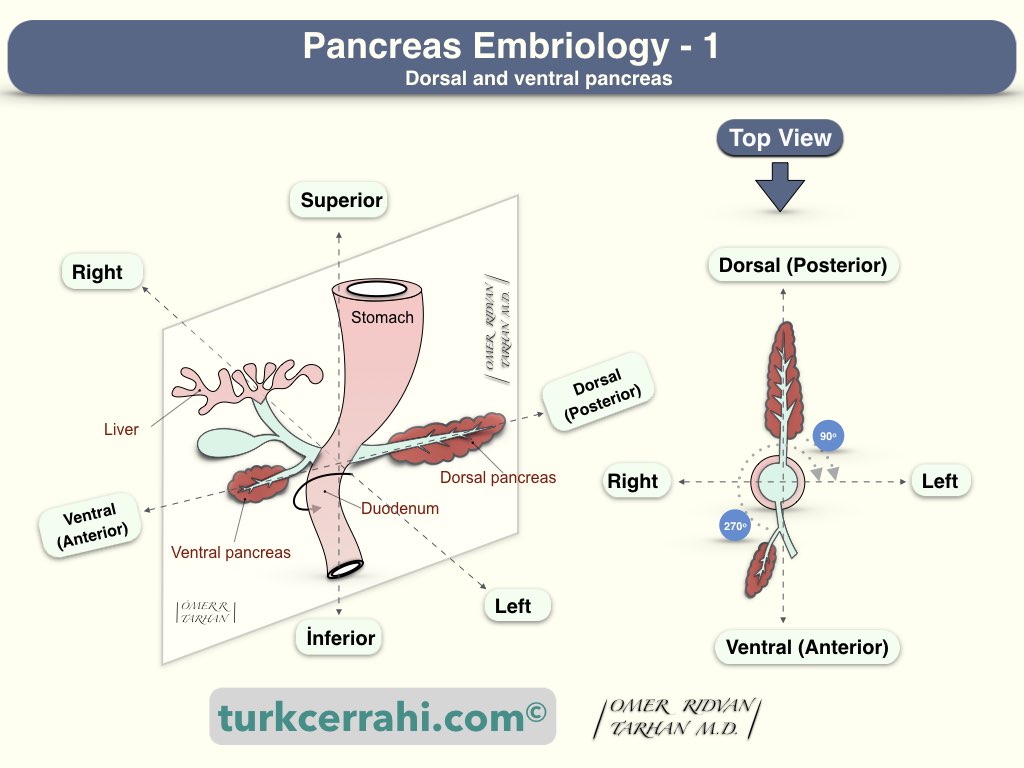
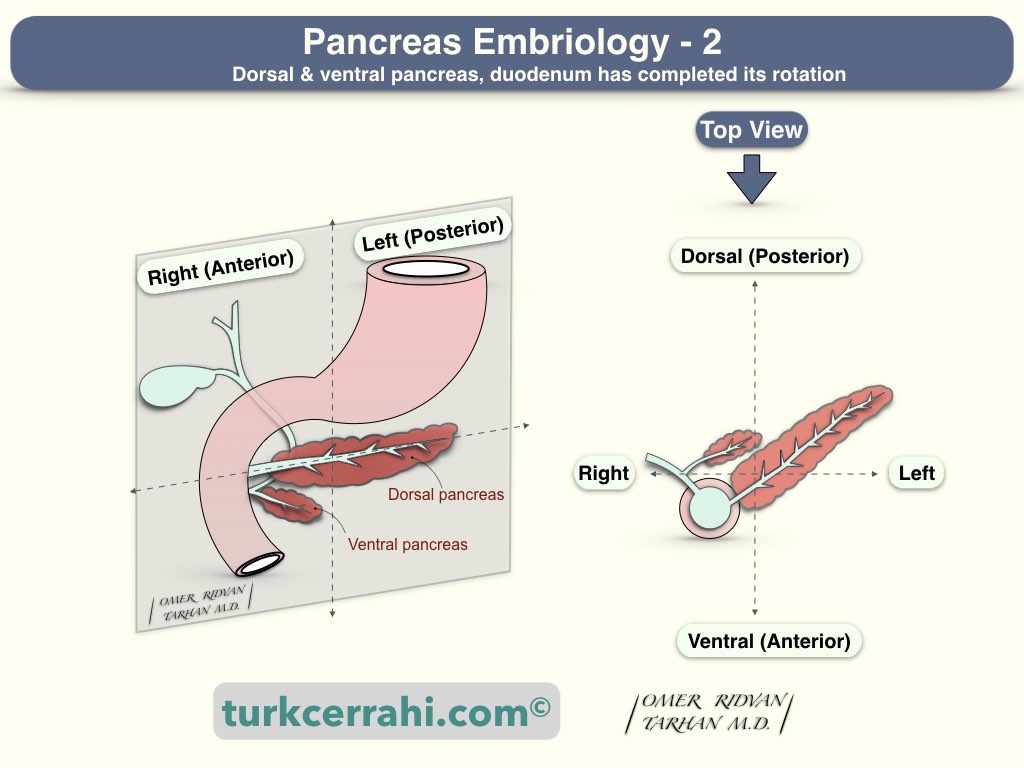
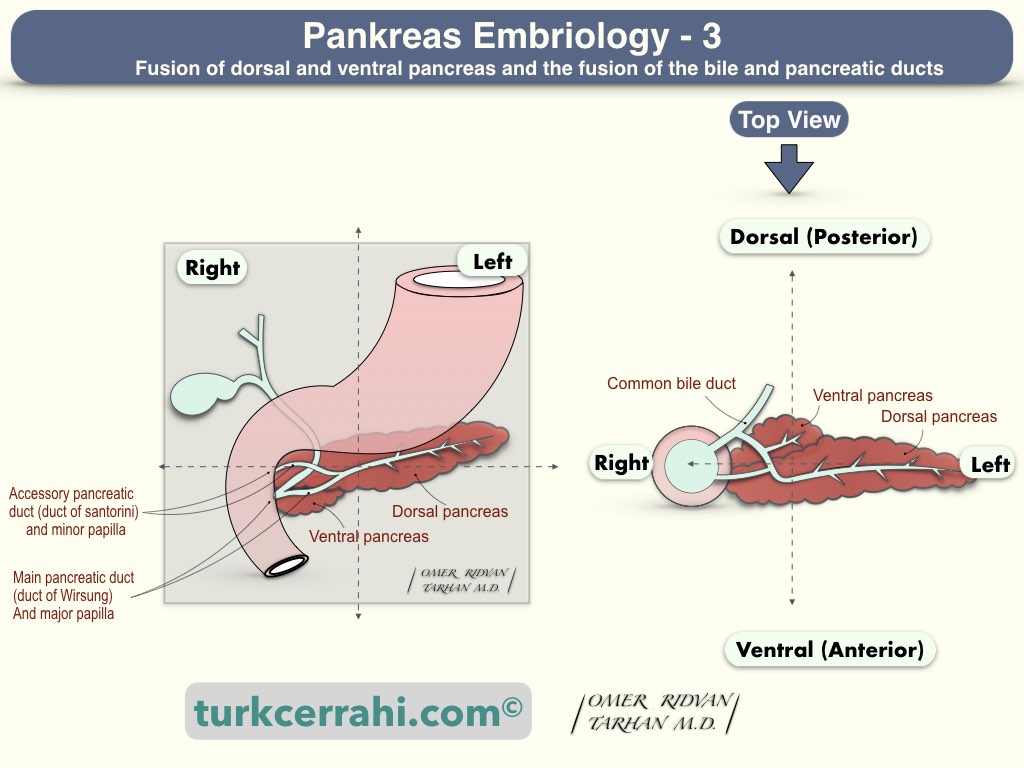
Understanding the anatomy and variations of the pancreatic ducts requires knowledge of pancreatic development.
The foregut used to be just a straight tube. The pancreas develops from ventral and dorsal pancreatic buds that are located anteriorly and posteriorly to the foregut, respectively. The foregut, from which the pancreas develops, will then elongate into a "C" shape and turn from the front to the right (duodenum). In the following period, the anterior bud (ventral pancreas) turns 270 degrees to the right of the duodenum, and the posterior bud (dorsal pancreas) turns 90 degrees to the right and unites.
Anatomic Variations of Pancreatic Ducts and Pancreas Divisum (Wirsung & Santorini)
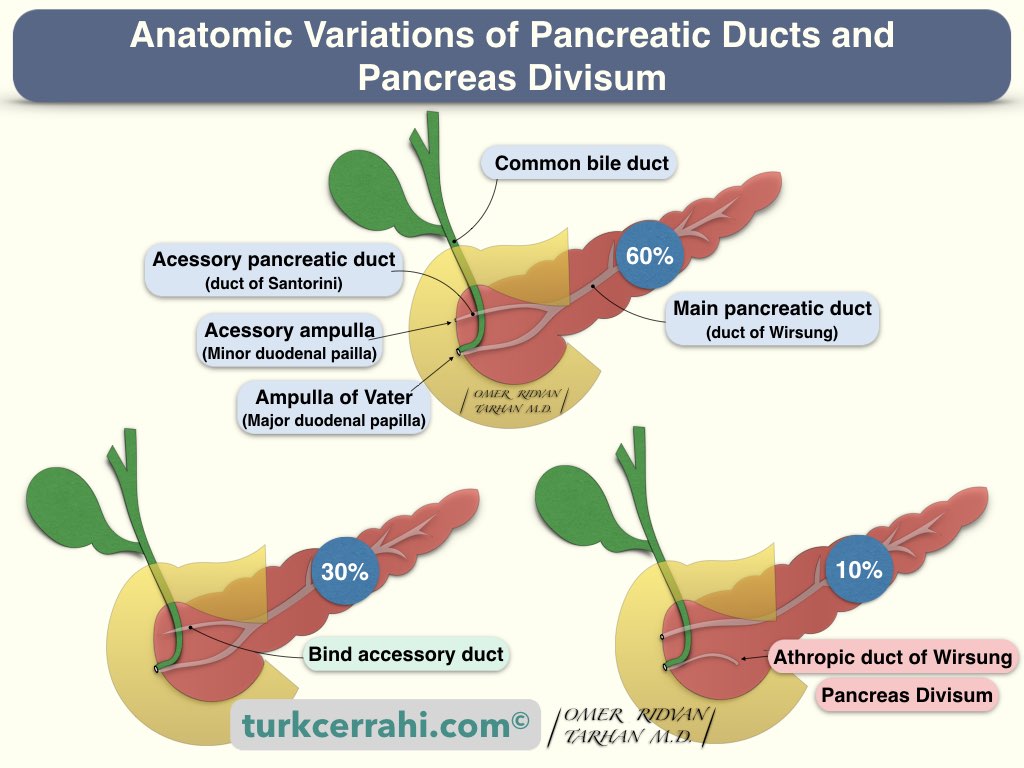
- The duct of the ventral pancreas joins with the duct of the dorsal pancreas to form the duct of Wirsung (major pancreatic duct) in the neck. The dorsal pancreatic duct remains as the Santorini duct (Minor, accessory pancreatic duct) (60%).
- Sometimes the duct of Santorini ends blindly and does not open into the duodenum (30%).
- Pancreas divisum: The duct of Wirsung and Santorini cannot unite, they open separately into the duodenum (In this case, most of the pancreas is drained from the minor duct (Duct of Santorini) (10%).
Anatomic Variations of Ampulla of Vater; Relations of Duct of Wirsung and Common Bile Duct
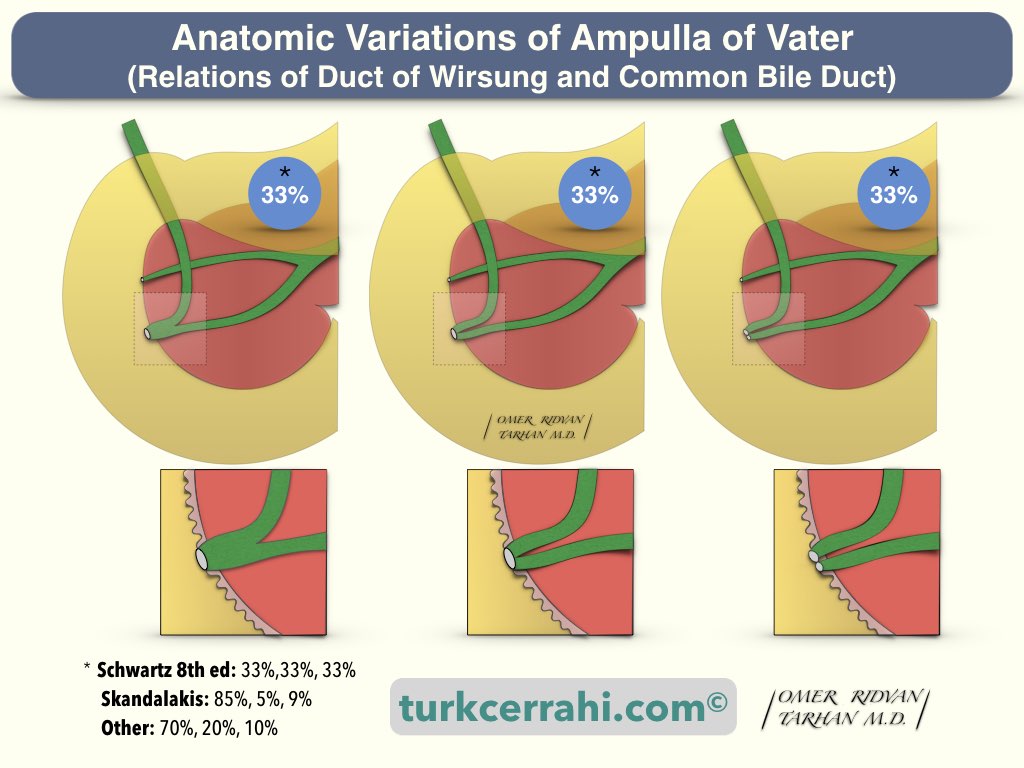
Typically, the main pancreatic duct (Wirsung) joins the common bile duct before opening into the duodenum (Y-shaped opening). In this case, there is a common canal and a true ampulla (Ampulla of Vater).
There are two more variations. In one, the two channels run separately but open to the duodenum from the same orifice (V-shaped opening).
In the third variation, the canals open separately into the duodenum (a U-shaped opening).
Y, V, and U-shaped opening rates are stated as ⅓, ⅓, ⅓ in Schwartz, 85%, 5%, and 9% in Scandalaks, and 70%, 20%, and 10% in some other sources.
Ampulla of Vater, Sphincter of Oddi, Papilla of Vater, Papilla Duodeni Minor
Ampulla of Vater (Hepatopancreatic Ampulla)
After the main pancreatic duct (Wirsung) and the common bile duct merge, they expand and open into the duodenum. This enlarged part is called the ampulla of Vater.
Sphincter of Oddi
The sphincter of Oddi (a smooth muscle) wrapped around the ampulla of Vater. It generates a resting pressure of 15-20 cm of water in the bile ducts and twice that in the pancreatic duct (in starvation). When we eat, this sphincter relaxes, the gallbladder contracts, and the bile is emptied into the food.
Papilla of Vater (Major Duodenal Papilla)
It is the elevation (projection) in the duodenum at the opening of the ampulla of Vater. It contains the sphincter of Oddi and the ampulla of Vater. The ampulla of Vater is located on the posteromedial aspect of the second portion of the duodenum. During the ERCP, the papilla of Vater is located, inserted, and cut (endoscopic sphincterotomy).
Minor Duodenal Papilla
The Santorini duct connects to the minor duodenal papilla, which is 1-2 cm proximal to the major duodenal papilla.
2. Arterial Supply of the Pancreas
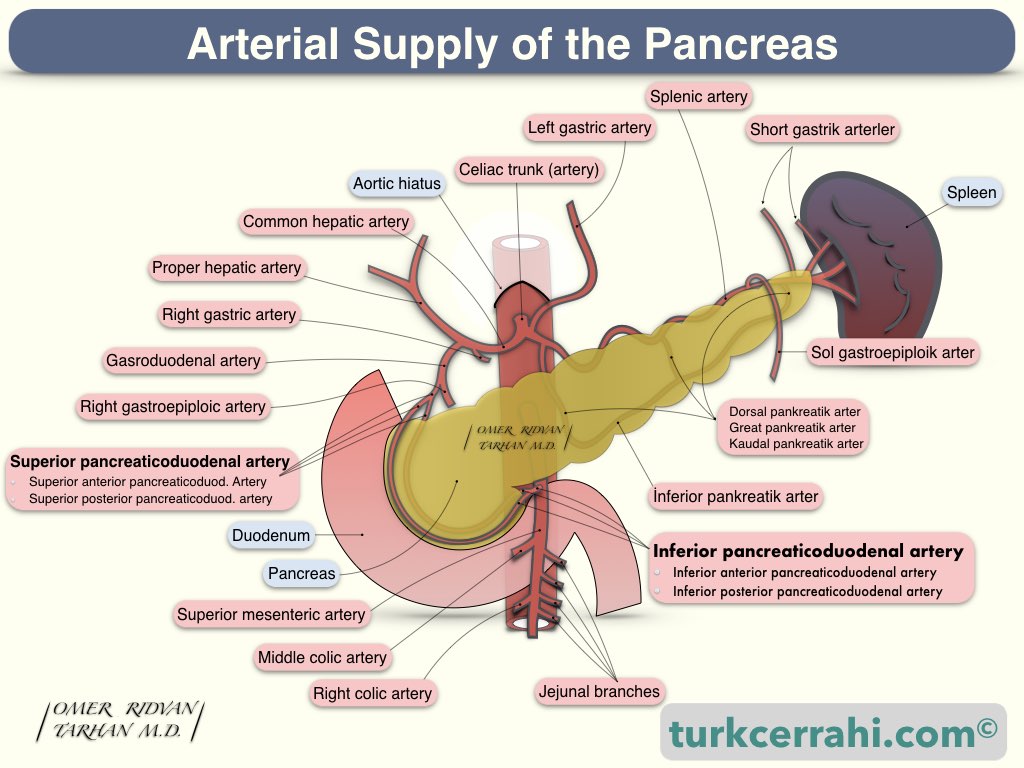
The pancreatic arteries come from both the celiac artery and the superior mesenteric artery.
First, the right gastric artery and then the gastroduodenal artery arise from the hepatic artery.
The gastroduodenal artery gives rise to the superior pancreaticoduodenal artery, which then divides into anterior and posterior branches.
The inferior pancreaticoduodenal artery emerges as the first branch from the superior mesenteric artery and divides into two (anterior and posterior) branches.
These branches anastomose with each other and even act as a continuation of each other. In other words, an anastomosis forms here between the celiac and superior mesenteric arteries. In cases of celiac artery occlusion (stenosis or thrombosis), the superior mesenteric artery can retrogradely supply blood.
Both the superior and inferior pancreaticoduodenal arteries have anterior and posterior branches that run close to the duodenal C near the pancreas head. They supply numerous branches to both the pancreatic head and the duodenum. As a result, it is impossible to separate the entire head of the pancreas from the duodenum without disrupting the duodenum's blood supply. The pancreas can be removed, leaving only the vessels and a small amount of pancreatic tissue (95% pancreatectomy).
The superior mesenteric artery (20%) can give rise to the right hepatic artery, called the replaced right hepatic artery. In some cases, the superior mesenteric artery also gives rise to the common hepatic artery. If the replaced right hepatic artery is not identified, it may be ligated inadvertently during the Whipple procedure.
The body and tail of the pancreas are supplied by splenic artery branches.
The inferior pancreatic artery arises from the superior mesenteric artery and runs parallel to the splenic artery along the posteroinferior border of the pancreas. The three perpendicular arteries bridge the splenic artery and the inferior pancreatic artery. These are the dorsal pancreatic artery, the great pancreatic artery, and the caudal pancreatic arteries (medial to lateral).
3. Venous Drainage of the Pancreas
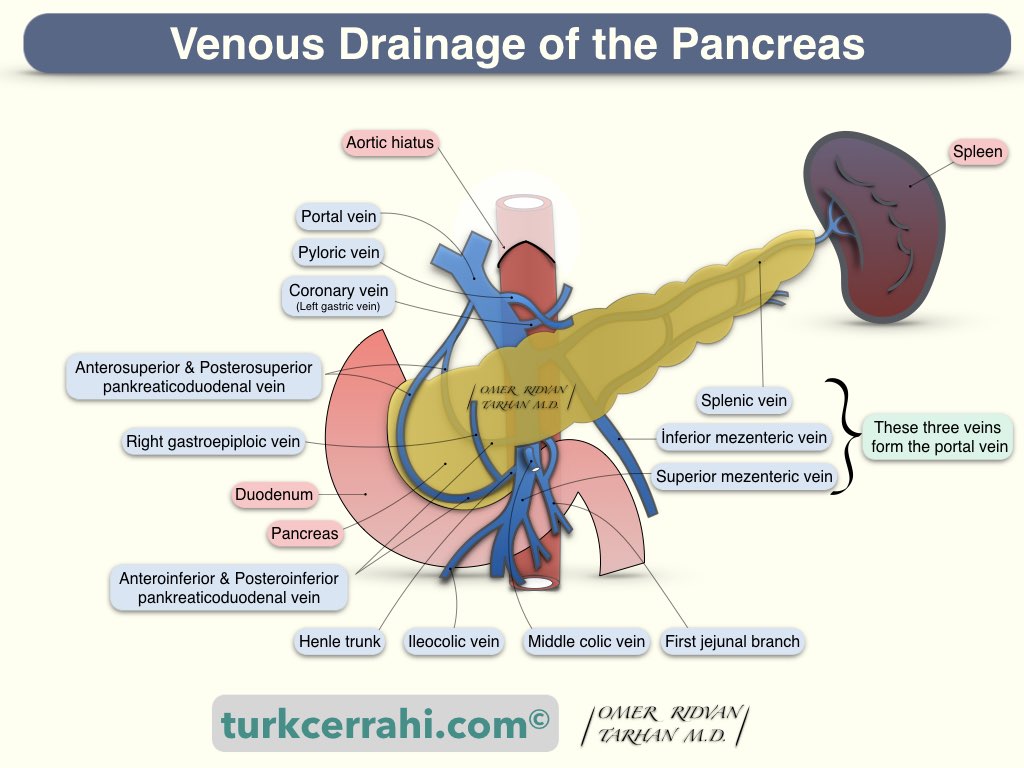
Comparable to arteries, the anterior and posterior pancreaticoduodenal veins are located in front of and behind the pancreatic head, respectively. They drain into the portal vein and the superior mesenteric vein. Venous blood from the body and tail of the pancreas empties into the splenic vein.
4. Lymphatic Drainage of the Pancreas
There is a diffuse and widespread lymphatic network. As a result, lymph nodes in pancreatic cancer are frequently invaded, and the local recurrence rate after resection is high. Lymphatic spread can occur along the lymph nodes of the superior mesenteric vein, hepatic artery, porta hepatis, transverse colon, and splenic vein.
5.Innervation of the Pancreas
The sympathetic nervous system increases endocrine (islet cells) and exocrine (acinar cells) secretions, while the parasympathetic nervous system decreases them.
Afferent sensory nerves are also abundant in the pancreas (part of the somatic system). Therefore, severe pain occurs in advanced pancreatic cancer and in acute and chronic pancreatitis.